
Transforming the understanding and treatment of mental illnesses.
Información en español

Research Funded by NIMH
Research conducted at nimh (intramural research program), priority research areas.
- Research Resources
The National Institute of Mental Health (NIMH), part of the National Institutes of Health (NIH), is the lead federal agency for research on mental disorders, supporting research that aims to transform the understanding and treatment of mental illnesses through basic and clinical research. Learn more about NIMH-funded research areas, policies, resources, initiatives, and research conducted by NIMH.
Notify the NIMH Press Team about NIMH-funded research that has been submitted to a journal for publication, and we may be able to promote the findings.

NIMH Strategic Plan
The NIMH Strategic Plan for Research outlines the Institute's research goals and priorities over the next five years. Learn more about the Strategic Plan.
NIMH supports research at universities, medical centers, and other institutions via grants, contracts, and cooperative agreements. Learn more about NIMH research areas, policies, resources, and initiatives:
- Research Domain Criteria (RDoC)
- Policies and Procedures
- Inside NIMH - Funding and Research News
The Division of Intramural Research Programs (IRP) is the internal research division of the NIMH. Over 40 research groups conduct basic neuroscience research and clinical investigations of mental illnesses, brain function, and behavior at the NIH campus in Bethesda, Maryland. Learn more about research conducted at NIMH:
- Intramural Investigators
- Intramural Research Groups
- Fellowships and Training
- Office of the Scientific Director
- Collaborations and Partnerships
- Join a Study
- IRP News and Events

- NIMH Priority Research Areas
- Highlighted Research Initiatives
Resources for Researchers
- Psychosocial Research at NIMH: A Primer
- Genomics Research Guidance for Grant Applicants
NIMH Women Leading Mental Health Research
Diversity in the scientific workforce enhances excellence, creativity, and innovation. NIMH and the National Institutes of Health (NIH) are committed to increasing diversity in the scientific workforce. Learn more about early-career women scientists whose NIMH-funded research is playing a role in advancing our mission of transforming the understanding and treatment of mental illnesses.

- Vision, Mission and Purpose
- Focus & Scope
- Editorial Info
- Open Access Policy
- Editing Services
- Article Outreach
- Why with us
- Focused Topics
- Manuscript Guidelines
- Ethics & Disclosures
- What happens next to your Submission
- Submission Link
- Special Issues
- Latest Articles
- All Articles
Childhood sexual abuse as a predictor of Complex Posttraumatic Stress Disorder: A meta-analysis
Marcelo Nvo-Fernández 1* , Valentina Miño-Reyes 1 , Gastón González-Cabeza 2 , Sofia Gálvez-Cienfuegos 1 , Martina Ignacia C.C 2 1 Laboratory of Methodology, Behavioural Sciences and Neuroscience, Faculty of Psychology, Universidad de Talca, Talca, Chile 2 Universidad Autónoma de Chile, Talca, Chile
Sexual abuse, especially when it occurs during childhood, is an experience that causes deep and lasting harm. Currently, its study as a risk factor for the development of trauma-related pathologies is of great relevance. In 2018, Complex Post-Traumatic Stress Disorder (CPTSD) was officially recognized as a distinct syndrome in the 11th Revision of the International Classification of Diseases (ICD-11), with the aim of distinguishing it from neurotic disorders secondary to stressful situations, somatoform disorders, and those specifically associated with stress. The inclusion of CPTSD in the ICD-11 marked the culmination of two decades of research dedicated to understanding its symptoms, treatments, and risk factors. This article aims to conduct a meta-analysis that explores the relationship between sexual abuse and the development of CPTSD. Fifteen studies were selected for analysis, and the results revealed several key risk factors associated with the development of CPTSD, with the primary one being childhood sexual abuse (k = 15; OR = 3.007).
Mood Disorders and Rapid Screening: A Brief Review
Helene Vossos 1* , Ozioma Nwosu-Izevbekhai 2 1 Associate Professor of Nursing, PMHNP Program Coordinator, University of St. Augustine for Health Sciences, St. Augustine, Florida, USA 2 Assistant Professor in Residence, University of Nevada, Las Vegas, USA
Objective: The purpose of this manuscript is for readers to understand the differences between bipolar and unipolar mood disorders. Readers will be able to apply evidence-based screening tools to differentiate in the diagnosis of bipolar versus unipolar depressive disorders. The goal is to increase diagnostic accuracy of mood disorders with the opportunity to provide treatment that will lead to improved patient outcomes.
Method: Review of literature discovered 13 articles that were pertinent with three major themes. One theme showed up to 62% of bipolar disorder cases were missed or undiagnosed upon the first evaluation, second theme showed 7% to 70% of individuals were misdiagnosed with adverse outcomes and third theme discovered the importance of specialty psychiatric training, education and the use of evidence-based screening tools combined with clinical judgement improved the accuracy of the correct mood disorder diagnosis.
Findings: In mood disorders, if left untreated or misdiagnosis occurs, the risk of suicide is higher (29.2%) in bipolar affective disorder, versus unipolar major depressive disorder (17.3%).
Implications for clinical practice: Recommendation for the use of evidence-based screening tools are clinical best practices for screening and diagnosing bipolar affective disorders with a statistical significance of 95%. Misdiagnosis is common up to 70% and the implications of timely rapid assessments allow for prompt interventions that has shown to halt and/or prevent mental health conditions to worsen, reducing risk of emergency situations.
Adolescents' Participation in Drug Addiction Interventions, Individual Perceptions, and Attitudes towards Recovery: A Scoping Review
Anthony Ezerioha 1 , Masoud Mohammadnezhad 2* 1 School of Allied Health and Social Care, Faculty of Health, Medicine and Social Care, Angelia Ruskin University, Cambridge, UK 2 Faculty of Health, Education and Life Sciences, School of Nursing and Midwifery, Birmingham City University, Birmingham, UK
Introduction : Adolescents recovering from substance use problems face significant psycho-social challenges. These challenges can affect their recovery progress, overall well-being, and integration into the society. Due to paucity studies, this study aimed to identify the perceptions and attitude towards recovery among adolescents participating in drug addiction interventions.
Methods : This systematic review study applied a complete search of relevant databases, including Scopus, Embase, Cinahl, and PubMed/Medline using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The search was limited to articles published in English language, between 2013 and 2023, and focused on adolescents drug addiction. Twelve articles were critically appraised using Critical Appraisal Skills Programme (CASP) for qualitative studies and Joanna Briggs Institute (JBI) tools. The results were synthesised using a thematic analysis.
Results: The findings identify that adolescents in addiction recovery face several challenges, including stigmatisation, social isolation, self-doubt, and difficulties accessing and maintaining treatment. The findings also point out that supportive relationships, culturally sensitive treatment approaches and interventions to combat self-stigma can play a critical role in promoting resilience and recovery for adolescents in recovery.
Conclusion : The comprehensive review brings us up to speed on the challenging experiences young people recovering from addiction in different addiction intervention go through, it underscores the importance of supportive relationships and encourages strengthening of interventions that mitigate against stigmatization.
Tele-Psychiatry to Address Severe Persistent Mental Illness in Rural Communities: An Economic and Break-Even Analysis
Sarah C. Haynes 1,2* , James P. Marcin 1,2 , Peter Yellowlees 3 , Stephanie Yang 1 , Jeffrey S. Hoch 4,5 1 Department of Pediatrics, University of California Davis, Sacramento, California, USA 2 Center for Health and Technology, University of California Davis, Sacramento, California, USA 3 Department of Psychiatry, University of California Davis, Sacramento, California, USA 4 Department of Public Health Sciences, University of California Davis, Sacramento, California, USA 5 Center for Healthcare Policy and Research, University of California Davis, Sacramento, California, USA
Background: People living in rural communities experience significant barriers accessing mental health care, including a shortage of psychiatrists and other behavioral health specialists. Telemedicine has the ability to improve access for these populations by allowing psychiatrists in urban settings to treat rural patients over video. However, start-up costs may hinder implementation of new tele-psychiatry programs.
Materials and Methods: We created a model to estimate the point at which tele-psychiatry would financially break even based on estimates of improved access to outpatient care for people with schizophrenia and bipolar disorder. We demonstrate how our model can be used with an example of a tele-psychiatry program serving five rural Indian Health Services clinics in California.
Results: When reimbursement for psychiatric services provided over telemedicine is relatively low compared to reimbursement for hospitalization visits, changes in the ratio of hospitalizations to telemedicine visits have very little impact on required hospitalization improvement.
Conclusions: Tele-psychiatry programs are likely to break even within the first three years when providing psychiatry services to a rural community with a scarcity of mental health services. Our findings are important because they indicate that the cost of improving access to tele-psychiatry services is likely low compared to the potential cost savings associated with reduced hospitalizations for people with severe persistent mental illness.
Barriers and Solutions to Comprehensive Care for Mental Health Patients in Hospital Emergency Departments
Elizabeth Levin 1* , Husam Aburub 2 1 Department of Psychology, Laurentian University, Sudbury, Ontario, Canada 2 Health Sciences North, Sudbury, Ontario, Canada
Hospital emergency departments in Ontario, have become a common place for patients with mental health problems to seek treatment. Studies report healthcare providers have limited knowledge and competency to provide optimal care for patients with mental health problems. As a result, these patients are at risk of poor hospital experiences and treatment outcomes. In addition, emergency staff report considering patients with mental health problems lower priority to other patients. This paper reviews the existing literature and examines the challenges surrounding patients with mental health problems seeking treatment in emergency rooms and how it leads to sub-optimal care. Strategies are then shared to overcome these challenges by changing emergency department experiences for mental health patients seeking treatment.
Effects of Interpersonal Psychotherapy on Postpartum Depression among Females at Tertiary Care Hospital Lahore
Sehrish Arshad 1* , Muhammad Afzal 2 , Hajra Sarwar 3 1 Doctors Hospital College of Nursing and Allied Health Sciences, Lahore, Pakistan 2 Director Academics Faculty of Allied Health Sciences, University of Lahore, Pakistan 3 University of Lahore, Pakistan
Introduction: Postpartum depression (PPD) is a major public health issue among females after giving birth to the baby, characterized by low mood, feeling of guilt and suicide. When left untreated, it has the potential for a profound negative impact on mothers, children and families. The efficacy of interpersonal psychotherapy (IPT) in addressing depression has been well-documented. However, the impact of IPT on PPD remains inadequately substantiated, particularly within the context of Pakistan, where data pertaining to its effectiveness remains limited.
Objective: The aim of study was to assess the level of depression in postpartum females and evaluate the effects of IPT on PPD among females at tertiary care hospital Lahore.
Methods: A Randomized controlled trial (RCT) was conducted at the Services Hospital Lahore from September 2021 to the same month in 2023. Subjects (n=110) were screened using the hamilton depression rating scale (HDRS) and divided equally in intervention group and control group to get eight sessions of individual based IPT versus routine care. Data was analyzed using SPSS version 21, intergroup comparison was done by Mann Whitney U test for intra group comparison Wilcoxon Signed Rank test was used, with 95% Confidence Interval (CI) and 5% level of significance. Significance of result showed with p value <0.05.
Results: Prevalence of PPD among female was observed 82%. Upon receiving IPT, females exhibited a statistically significant reduction (p<0.001) in scores indicative of mild depression, from 48 (87.3%) to 5(9.1%), as well as for moderate depression, from 7(12.7%) to 1(1.8%). Furthermore, following the IPT sessions, marked improvements were noted within the intervention group across various domains including depressed mood p<0.001, CI (0.000, 0.027), feelings of guilt p<0.001, CI (0.000, 0.027), early night insomnia p<0.008, CI (0.000, 0.043), impaired work and activities p<0.05, CI (0.072, 0.200), and insight p<0.001, CI (0.000, 0.027). Conversely, the control group did not exhibit any significant alterations in these parameters.
Conclusion: The results indicate a concerning prevalence rate of PPD among the study sample with many cases remaining undiagnosed and untreated. More positively, the study demonstrates the potential of IPT as an effective method to mitigate mild to moderate PPD. This research suggests the incorporation of IPT into therapeutic models could result in timely, potentially preventive interventions and lessen the occurrence of severe complications.
Sex Differences in the Relationship Between Nucleus Accumbens Volume and Youth Tobacco or Marijuana Use Following Stressful Life Events
Shervin Assari 1,2,3 *, Payam Sheikhattari 4,5,6 1 Department of Internal Medicine, Charles R. Drew University of Medicine and Science, Los Angeles, CA, USA 2 Department of Family Medicine, Charles R. Drew University of Medicine and Science, Los Angeles, CA, USA 3 Department of Urban Public Health, Charles R. Drew University of Medicine and Science, Los Angeles, CA, USA 4 Center for Urban Health Disparities Research and Innovation, Morgan State University, Baltimore, MD, USA 5 The Prevention Sciences Research Center, School of Community Health and Policy, Morgan State University, Baltimore, MD, USA 6 Department of Public and Allied Health Sciences, School of Community Health and Policy, Morgan State University, Baltimore, MD, USA
Background: Exposure to stressful life events (SLEs) can upset balance and affect the healthy brain development of children and youths. These events may influence substance use by altering brain reward systems, especially the nucleus accumbens (NAc), which plays a key role in motivated behaviors and reward processing. The interaction between sensitization to SLEs, depression, and substance use might vary between male and female youths, potentially due to differences in how each sex responds to SLEs.
Aims: This study aims to examine the effect of sex on the relationship between SLEs, Nucleus Accumbens activity, and substance use in a nationwide sample of young individuals.
Methods: We utilized data from the Adolescent Brain Cognitive Development study (ABCD), a longitudinal study of pre-adolescents aged 9–10 years, comprising 11,795 participants tracked over 36 months. Structured interviews measuring SLEs were conducted using the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS). Initial linear regression analyses explored if SLEs could predict volumes of the right and left NAc. Subsequently, Cox regression models were used to investigate how SLEs and NAc volume might predict the initiation of tobacco and marijuana use, with the analysis stratified by sex to address potential sex differences.
Results: Our findings reveal that SLEs significantly predicted marijuana use in males but not in females, and tobacco use was influenced by SLEs in both sexes. A higher number of SLEs was linked with decreased left NAc volume in males, a trend not seen in females. The right NAc volume did not predict substance use in either sex. However, volumes of both the right and left NAc were significant predictors of future tobacco use, with varying relationships across sexes. In females, an inverse relationship was observed between both NAc volumes and the risk of tobacco use. In contrast, a positive correlation existed between the left NAc volume and tobacco and marijuana use in males, with no such relationship for females.
Conclusion: This study underscores that the associations between SLEs, NAc volume, and subsequent substance use are influenced by a nuanced interplay of sex, brain hemisphere, and substance type.
What is Common Becomes Normal; Black-White Variation in the Effects of Adversities on Subsequent Initiation of Tobacco and Marijuana During Transitioning into Adolescence
Shervin Assari 1,2* , Babak Najand 3 , Payam Sheikhattari 4,5,6 1 Department of Internal Medicine, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA 2 Department of Urban Public Health, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA 3 Marginalization-related Diminished Returns Center, Los Angeles, CA, USA 4 Center for Urban Health Disparities Research and Innovation, Morgan State University, Baltimore, MD, USA 5 The Prevention Sciences Research Center, School of Community Health and Policy, Morgan State University, Baltimore, MD, USA 6 Department of Behavioral Health Science, School of Community Health and Policy, Morgan State University, Baltimore, MD, USA
Background: While adversities across domains of finance, race, family, and life may operate as risk factors for initiation of substance use in adolescents, the influence of these factors may vary across racial groups of youth. Unfortunately, the existing knowledge is minimal about racial differences in the types of adversities that may increase the risk of subsequent substance use initiation during the transition into adolescence.
Aim: To compare racial groups for the effects of adversities across domains of finance, race, family, and life on subsequent substance use initiation among pre-adolescents transitioning into adolescence.
Methods: In this longitudinal study, we analyzed data from 6003 non-Latino White and 1562 non-Latino African American 9-10-year-old children transitioning into adolescence. Data came from the Adolescent Brain Cognitive Development (ABCD) study. Participants were followed for up to thirty-six months as they transitioned to adolescence. The independent variables were adversities related to the domains of finance, race, family, and life. The primary outcomes were time to first tobacco or marijuana use. Age, puberty, and gender were confounders. Cox regression models were used for data analysis.
Results: For White youth, tobacco use was under influence of having two parents in the household (HR = .611; 95% CI = .419-.891), parental education (HR = .900; 95% CI = .833-.972), household income (HR = .899; 95% CI = .817-.990), racial stress (HR = 1.569; 95% CI = 1.206-2.039), and life stress (HR =1.098 ; 95% CI = 1.024-1.178) and marijuana use was under influence of neighborhood income (HR = .576; 95% CI = .332-.999) and financial stress (HR =4.273; 95% CI = 1.280-17.422). No adverse condition predicted tobacco or marijuana use of African American youth.
Conclusion: The effects of adversities on substance use depend on race. While various types of adversities tend to increase subsequent initiation of tobacco and marijuana, such factors may be less influential for African American adolescents, who experience more of such adversities. What is common may become normal.
Diagnosing Human Trafficking Victims: A Mini-Review and Perspective
Sheldon X. Zhang 1 , Rumi Kato Price 2* 1 School of Criminology and Criminal Justice Studies, University of Massachusetts at Lowell, Lowell, Massachusetts, USA 2 Department of Psychiatry, School of Medicine, Washington University in St. Louis, St. Louis, Missouri, USA
The global campaign against human trafficking, also known as trafficking in persons, has gained much momentum in the past two decades. Although psychiatric and physical illness sequela of human trafficking are well documented, the research community continues to struggle over such foundational questions as what specific activities or experiences count as trafficking-in-persons victimization and how best to obtain representable and generalizable data on experiences of people who are trafficked. We provide a brief review of major efforts to define trafficking in persons to establish prevalence estimates to date. We argue for consensus on key clinical and public health indicators, resembling the Diagnostic and Statistical Manual (DSM) approach to enable common and systematic knowledge building and comparability across studies.
Immigration, Educational Attainment, and Subjective Health in the United States
Rifath Ara Alam Barsha 1 , Babak Najand 2 , Hossein Zare 3,4 , Shervin Assari 5,6,7* 1 School of Community Health & Policy, Morgan State University, Baltimore, MD, USA 2 Marginalization Related Diminished returns, Los Angeles, CA, USA 3 Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA 4 University of Maryland Global Campus, Health Services Management, Adelphi, Maryland, USA 5 Department of Family Medicine, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA 6 Department of Internal Medicine, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA 7 Department of Urban Public Health, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA
Objectives: Although educational attainment is a major social determinant of health, according to Marginalization-related Diminished Returns (MDRs), the effect of education tends to be weaker for marginalized groups compared to the privileged groups. While we know more about marginalization due to race and ethnicity, limited information is available on MDRs of educational attainment among US immigrant individuals.
Aims: This study compared immigrant and non-immigrant US adults aged 18 and over for the effects of educational attainment on subjective health (self-rated health; SRH).
Methods: Data came from General Social Survey (GSS) that recruited a nationally representative sample of US adults from 1972 to 2022. Overall, GSS has enrolled 45,043 individuals who were either immigrant (4,247; 9.4%) and non-immigrant (40,796; 90.6%). The independent variable was educational attainment, the dependent variable was SRH (measured with a single item), confounders were age, gender, race, employment and marital status, and moderator was immigration (nativity) status.
Results: Higher educational attainment was associated with higher odds of good SRH (odds ratio OR = 2.08 for 12 years of education, OR = 2.81 for 13-15 years of education, OR = 4.38 for college graduation, and OR = 4.83 for graduate studies). However, we found significant statistical interaction between immigration status and college graduation on SRH, which was indicative of smaller association between college graduation and SRH for immigrant than non-immigrant US adults.
Conclusions: In line with MDRs, the association between educational attainment and SRH was weaker for immigrant than non-immigrant. It is essential to implement two sets of policies to achieve health inequalities among immigrant populations: policies that increase educational attainment of immigrants and those that increase the health returns of educational attainment for immigrants.
Commentary: Black Mothers in Racially Segregated Neighborhoods Embodying Structural Violence: PTSD and Depressive Symptoms on the South Side of Chicago
Loren Henderson 1* , Ruby Mendenhall 2 , Meggan J Lee 3 1 The School of Public Policy, University of Maryland, Baltimore County, Baltimore, MD, USA 2 Department of Sociology, Department of African American Studies, Carle Illinois College of Medicine, IL, USA 3 Carle Illinois College of Medicine, Urbana, IL, USA
Exposure to Adverse Life Events among Children Transitioning into Adolescence: Intersections of Socioeconomic Position and Race
Shervin Assari 1,2,3* , Babak Najand 4 , Alexandra Donovan 1 1 Department of Internal Medicine, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA 2 Department of Family Medicine, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA 3 Department of Urban Public Health, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA 4 Marginalization related Diminished Returns Center, Los Angeles, CA, USA
Background: Racism is shown to diminish the protective effects of family socioeconomic position (SEP) resources for racial minorities compared to the majority groups, a pattern called minorities’ diminished returns. Our existing knowledge is minimal about diminished returns of family SEP indicators on reducing exposure to adverse life events among children transitioning into adolescence. Aim: To compare diverse racial groups for the effects of family income and family structure on exposure to adverse life events of pre-adolescents transitioning to adolescence.
Methods: In this longitudinal study, we analyzed data from 22,538 observations belonging to racially diverse groups of American 9–10-year-old children (n = 11,878) who were followed while transitioning to adolescence. The independent variables were family income and family structure. The primary outcome was the number of stressful life events with impact on adolescents, measured by the Life History semi-structured interview. Mixed-effects regression models were used for data analysis to adjust for data nested to individuals, families, and centers.
Results: Family income and married family structure had an overall inverse association with children’s exposure to adverse life events during transition to adolescence. However, race showed significant interactions with family income and family structure on exposure to adverse life events. The protective effects of family income and married family structure were weaker for African American than White adolescents. The protective effect of family income was also weaker for mixed/other race than White adolescents.
Conclusion: While family SEP is protective against children’s exposure to adverse life events, this effect is weaker for African American and mixed/other race compared to White youth.
Generalized Anxiety Disorder and Depression Associated with Developmental Prosopagnosia: A Case Report
Kaishi Imatani 1 , Takeshi Inoue 2* , Yuji Oto 1 , Tasuku Kitajima 2 , Ryoko Otani 2 , Satoshi F Nakashima 3 , So Kanazawa 4 , Masami K. Yamaguchi 5 , Ryoichi Sakuta 2 , Tomoyo Matsubara 1 1 Department of Pediatrics, Dokkyo Medical University Saitama Medical Center, Koshigaya, Saitama, Japan 2 Child Development and Psychosomatic Medicine Center, Dokkyo Medical University Saitama Medical Center, Koshigaya, Saitama, Japan 3 Department of Psychological Sciences, University of Human Environments, Okazaki, Aichi, Japan 4 Department of Psychology, Japan Women’s University, Kawasaki, Kanagawa, Japan 5 Department of Psychology, Chuo University, Hachioji, Tokyo, Japan
Developmental prosopagnosia is a disorder of facial recognition that begins during early childhood in the absence of acquired central nervous system disease. We report the case of a 15-year-old female with developmental prosopagnosia as measured by the 20-item Prosopagnosia Index and Cambridge Face Memory Test who ultimately developed generalized anxiety disorder and depression despite relatively normal social and psychological function during early childhood. In elementary school, the case patient adapted by learning alternative ways to identify others, such as by clothing and hairstyle, but this became more difficult in junior high school due to the requirement for school uniforms and regulations on hairstyle. This difficulty in turn led to interpersonal problems that ultimately resulted in symptoms of generalized anxiety disorder and depression, such as headache and sleep dysfunction. People with developmental prosopagnosia are generally prone to having depressed and anxious feelings. However, to the best of our knowledge, this is the first case report of anxiety disorder or depression related to developmental prosopagnosia. This comorbidity may be relatively common, especially in ethnically homogeneous countries with strict school regulations on personal appearance such as Japan.
Remote Warfare with Intimate Consequences: Psychological Stress in Service Member and Veteran Remotely-Piloted Aircraft (RPA) Personnel
Seth Davin Norrholm 1,2* , Jessica L. Maples-Keller 3 , Barbara O. Rothbaum 3 , Chad C. Tossell 2 1 Neuroscience Center for Anxiety, Stress, and Trauma, Department of Psychiatry and Behavioral Neurosciences, Wayne State University School of Medicine, Detroit, Michigan, USA 2 Department of Behavioral Sciences and Leadership, United States Air Force Academy, Colorado Springs, Colorado, USA 3 Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, Georgia, USA
The use of remote piloted aircraft (RPAs) has been a part of military operations for decades and this type of service can present its own unique constellation of combat experiences and psychological consequences. The RPA crewmember experience has typically involved surveillance, targeting, striking, and after-battle assessments of individuals of interest to a host country or agency from a distance that can span several thousand miles. These operators are engaged in physically remote activities that carry a significant degree of intimacy due to the live, high-resolution, high-fidelity images and sounds that are available to the combatants in real-time. The potential psychological consequences of this type of military occupational specialty can include the symptoms of depression, anxiety, and posttraumatic stress disorder (PTSD) as well as moral injury, mental exhaustion or burnout, and disturbed sleep. The following narrative review examines the current state of RPA warfare from a psychological trauma perspective with an emphasis on the evolution of the inherent technology, the operator force, the psychological experiences and consequences of this type of service, and potential preventative interventions for servicemembers. A key objective of this narrative review is to integrate the available peer-reviewed empirical data, experiential military perspectives and analyses, clinician observations from this unique population, and exemplar reports from those with lived experience on an RPA crew regarding psychological consequences of this military occupational specialty.
Social Anxiety in University Students: Towards an Intentional Life-Skills Based Prevention Model
Hannah Ali * , Steve Joordens Department of Psychology, University of Toronto Scarborough, Toronto, ON, Canada
Research suggests that staying connected with people is very beneficial to our physical and mental well-being. Moreover, a lack of social connection is associated with poor mental and physical health, and lower overall well-being. For individuals with social anxiety, it is particularly difficult to cultivate social connections. Due to the prolonged period of social isolation during the COVID-19 pandemic, research suggests that social anxiety in university students has increased. This study employed a convergent parallel mixed method design and administered a self-reported questionnaire which included quantitative and qualitative questions. The questionnaire was administered to 301 undergraduate students to determine if feelings of social anxiety in students changed during and after the pandemic. This study also analyzed social anxiety levels across racial and ethnocultural demographics and assessed the cultural stigmas and barriers that may prevent students from accessing mental health services. Results from the quantitative analyses showed a significant difference in social anxiety scores before and after the pandemic. However, in our sample, feelings of social anxiety post-pandemic did not differ across race, or income which were our main variables of interest. In addition, there was a positive correlation between social anxiety scores and household income and fear of negative evaluation. The qualitative results showed that important barriers to accessing mental health services include fear of parents learning they are in therapy, cost of mental health services, language barriers, and concern that a therapist would not have cultural sensitivity. This study highlights the need for increased interventions to reduce social anxiety among students, and proposes a preventative approach we refer to as “Life-Skills Training” to address social anxiety.
Mental health clinical exams’ evident adherence to industry standards for testing
Benjamin E. Caldwell California State University Northridge, CA, USA
The developers of clinical exams for US mental health licensure have faced significant recent criticism and calls for their exams to be paused or discontinued. 1,2 Critics cite concerns over exams lacking evidence of validity, while they demonstrate strong evidence of racial and ethnic bias. Developers, in turn, argue that their exams are developed using accepted methods that conform with industry standards, specifically, the Standards for Educational and Psychological Testing . 3
This manuscript challenges that assertion. Based on external research as well as developers’ own statements and publications, clinical exams for US mental health care licensure appear to deviate in important ways from both the letter and the spirit of the Standards . Clinical exams should be paused unless and until they are shown to be fair, equitable, valid, and more fully consistent with industry norms.
Adolescent Woes? Approval Motivation, Test Anxiety, and the Role of Perceived Self-Control
Swati Y Bhave * , Jill N Mota, Latika Bhalla, Shailaja Mane, Anuradha Sovani, Surekha Joshi Association of Adolescents and Child Care in India (AACCI), India
The Association of Adolescents and Child Care in India (AACCI) conducts multicentric studies on youth behavior in India. Using openly accessible psychometric tools, the present study discusses the demographic-wise interrelationships between the Children’s Perceived Self-Control (PSC), Martin-Larsen Approval Motivation (AM), and Friedben’s Test Anxiety Scales (FTAS) administered to 712 students (Group-1: 10-14 yrs.; Group-II: 15-18 yrs.) from two Delhi-based schools. The survey-questionnaire included four demographic variables: age, gender, sibling status, and body mass index. Although mainstream literature has uniformly contented in favour of the benefits of PSC, one-way ANOVAs in the present study revealed that high PSC was associated with significantly high AM (F[2,709] =3.033, p =0.049), suggesting that people with high PSC may diligently weigh short- and long-term consequences, choosing behaviors that best align with their interests and enduringly valued goals. Further, this relationship was statistically significant for participants in the no siblings (p =0.005) and underweight groups (p =0.031). Participants with high PSC had the lowest FTAS scores; however, this relationship was not statistically significant. Lastly, AM and FTAS were negatively correlated (r =-0.216, p<0.01), especially for females, Group-II, and participants with siblings (r =-0.278, -0.292, and -0.244, respectively), clarifying distinct differences between AM and FTAS’ subscales. The implications of findings were shared with the school management to conduct customized interventions using the WHO’s Life Skills Education framework. The findings highlight the need for time-series interventional analysis to ascertain the direct and cumulative effects of intervention on the interrelationships between PSC, AM, and FTAS.
Increasing Diversity and Inclusion in Research on Virtual Reality Relaxation: Commentary on ‘Virtual Reality Relaxation for People with Mental Health Conditions: A Systematic Review’
Simon Riches 1,2,3* , Deanna Fallah 3,4 , Ina Kaleva 5 1 Department of Psychology, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London, United Kingdom 2 Social, Genetic & Developmental Psychiatry Centre, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London, United Kingdom 3 South London and Maudsley NHS Foundation Trust, London, United Kingdom 4 School of Psychology, University of Surrey, Surrey, United Kingdom 5 Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London, United Kingdom
The Effectiveness of Mentalization-Based Treatment on Mindfulness and Perceived Social Support in Adolescents
Sarah Bagherzadeh Jalilvand * , Sedigheh Ahmadi Department of Psychology and Educational Sciences, Kharazmi University, Tehran, Iran
Adolescence is a critical period marked by significant changes in social relationships and emotional development. In light of the importance of promoting mental health in this age group, this study aimed to investigate the effectiveness of a mentalization-based treatment intervention on mindfulness and perceived social support among female adolescents aged 12-15 years in Tehran.
A pretest-posttest control group design was employed, with participants randomly assigned to either the intervention group, which received the mentalization-based treatment, or the control group, serving as a comparison for evaluating the intervention's effectiveness. The Mindful Attention Awareness Scale (MAAS) and the Multidimensional Scale of Perceived Social Support Questionnaire (MSPSS) were used to measure mindfulness and perceived social support, respectively.
The mentalization-based treatment intervention focused on enhancing the participants' ability to understand and interpret their own and others' mental states, fostering empathy, and improving interpersonal relationships.
Data analysis was performed using Multivariate Analysis of Covariance (MANCOVA) to assess the impact of the mentalization-based treatment on mindfulness and perceived social support in female adolescents. The results indicated a significant improvement in both mindfulness and perceived social support after the intervention (P < 0.01).
In conclusion, the findings suggest that mentalization-based treatment holds promise as an effective approach to enhance mental health outcomes, particularly in promoting mindfulness and perceived social support in female adolescents. Future attention should be given to the implementation of this intervention to support the well-being of adolescents during this critical developmental stage.
Race, Socioeconomic Status, Health Locus of Control, and Body Mass Index
Shervin Assari 1,2,3,4 *, Babak Najand 5 1 Department of Urban Public Health, Charles R. Drew University of Medicine and Science, Los Angeles, CA, USA 2 Department of Family Medicine, Charles R. Drew University of Medicine and Science, Los Angeles, CA, USA 3 School of Nursing, Charles R. Drew University of Medicine and Science, Los Angeles, CA, USA 4 Department of Internal Medicine, Charles R. Drew University of Medicine and Science, Los Angeles, CA, USA 5 Marginalization-Related-Diminished Returns (MDRs) Center, Los Angeles, CA, USA
Background: This cross-sectional study aimed to investigate the complex interplay between socioeconomic status (SES), internal and external health locus of control, and body mass index (BMI) in a national sample of US adults. Given the unique challenges faced by Black individuals, it was hypothesized that the relationships between SES, internal and external health locus of control, and BMI would be weaker for Blacks compared to Whites.
Methods: For this cross-sectional study, baseline data from the MIDUS Refresher sample, consisting of US adults, were analyzed. SES indicators such as income and education were examined as predictors of internal and external health locus of control. The analyses were conducted overall without and with race interactions. We also ran models within different racial groups.
Results: Overall, 3198 participants entered our analysis who were White or Black. From this number, 2925 (91.5%) were White and 273(8.5%) were Black. In the pooled sample, high education and income were linked to higher internal and lower external health locus of control and lower BMI. The study revealed that the relationships between high SES indicators (income and education), internal health locus of control, and BMI were weaker for Black than White individuals. The study revealed that the relationships between high SES indicators (income and education) and external health locus of control was stronger for Black than White individuals.
Conclusion: This study provides evidence for the complex interrelationships between SES, health locus of control, and BMI, while highlighting the role of race as a moderating factor. The findings suggest that the effects of SES on internal health locus of control is influenced by race, with weaker relationships observed among Black individuals compared to Whites.
The Association Between Depression, Anxiety and COVID-19 Symptoms
Marilyn M. Bartholmae 1,2* , Joshua, M. Sill 3 , Matvey V. Karpov 1 , Sunita Dodani 1,4 1 EVMS-Sentara Healthcare Analytics and Delivery Science Institute, Norfolk, VA, USA 2 Department of Psychiatry and Behavioral Sciences, Eastern Virginia Medical School, Norfolk, VA, USA 3 Division of Pulmonology, Department of Internal Medicine, Eastern Virginia Medical School, Norfolk, VA, USA 4 Division of Cardiology, Department of Internal Medicine, Eastern Virginia Medical School, Norfolk, VA, USA
Background: The variation of COVID-19 illness is not fully understood. There is a need for further identification of predictors for COVID-19-related health outcomes, which may improve the delivery of healthcare. The primary objective was to identify whether anxiety/depression symptoms are associated with the number of COVID-19 symptoms. The second objective was to examine differences in anxiety and depression symptoms between individuals with or without COVID-19 symptoms.
Methods: 782 Virginians ages 18 to 87 years, enrolled from March to May 2021 and were followed-up for six months. Vibrent Health online platform was used to collect data. PHQ-9, GAD-7, and CDC's COVID-19 tracing form, were used to assess depression, anxiety, and COVID-19 symptoms, respectively. An MMRM test was used to examine whether anxiety and depression symptoms were associated with the number of COVID-19 symptoms. Age, race, sex, medical diagnoses, and COVID-19 related economic/social hardships were included as covariates. Mann-Whitney U tests were used to assess differences in anxiety/depression at all study time points. We conducted analyses using SAS 9.4, p- values < .05 were considered significant.
Results: Depression/anxiety symptoms, COVID-19 related economic/social hardships, and medical diagnoses, were significantly associated with the number of COVID-19 symptoms ( p <.05), whereas age, sex, and race were not ( p >.05). Overall, PHQ9 and GAD7 scores were consistently and significantly higher for individuals with COVID-19 symptoms than those without COVID-19 symptoms ( p <.05).
Conclusions: The severity of depression and anxiety symptoms is linked to symptoms of COVID-19 over time. Physical and mental health integrated healthcare approaches may be necessary. Further investigation into causative mechanisms is needed.
Does Mental Health impact the outcomes of Total Ankle Arthroplasty? A Systematic Review
Margaret A. Sinkler 1* , Amir H. Karimi 2 , Mohamed E. El-Abtah 2 , John E. Feighan 1 , Ethan R. Harlow 1 , Heather A. Vallier 2 1 University Hospitals, Case Western Reserve University, Cleveland, OH, USA 2 Case Western Reserve University School of Medicine, Cleveland, OH, USA
Studies have demonstrated that depression, anxiety, negative mood, and pain catastrophizing influence outcomes following total hip, knee, and shoulder arthroplasty thus providing evidence-based counseling on expected postoperative outcomes. The purpose of this review is to establish the prevalence of mental health conditions, impact of mental health conditions on patient-reported outcome measures, and the impact on length of stay and discharge disposition in patients undergoing total ankle arthroplasty (TAA). An online search utilizing the Cochrane Central Register of Controlled Trials, PubMed, Google Scholar, and CINAHL databases was performed to identify relevant articles published between 2010 and 2022. Seven studies were included in the systematic review. Depression was the most common mental health comorbidity with a pooled prevalence of 12.9%. Mental health comorbidities were associated with inferior patient reported outcomes measures. Additionally, depression was a pre-operative predictive factor in poor outcomes when utilizing the PROMIS score. The presence of a mental health comorbidity demonstrated an increased risk of nonhome discharge, length of stay, complication rate, infection, and narcotic use. Psychiatric comorbidities, particularly depression, were predictors of negative postoperative outcomes. This review reinforces the significant impact of mental health disorders and psychiatric comorbidities on clinical outcomes following TAA.
Level of Evidence: Level III
The Impact of COVID-19 on the Mental Health of the Western Populace: A Model for the Examination of the Virus’s Global Impacts on Mental Health
Watson Kemper 1 , Katie Ben-Judah 2 , Akamu J. Ewunkem 3 , Uchenna B. Iloghalu 2* 1 Department of Biology, North Carolina A & T State University, Greensboro, NC, USA 2 Department of Biology, Guilford College, Greensboro, NC, USA 3 Department of Biological Sciences, Winston-Salem State University, Winston-Salem, NC, USA
COVID-19 has had lasting impacts on the physical and mental health of the global community. These impacts are multifaceted and spring from a range of physiological, psychological, economic origins. This review sought to demonstrate evidence of the damaging consequences that COVID-19 and its related effects have had on mental health. The findings showed significant increases in numbers of individuals seeking mental health care, experiencing negative mental health symptoms, and opting for medication management of mental health symptoms. In this review, we explore logistical aspects of both present and prospective zoonotic disease spillover events, as this information is key to mitigating future pandemic events. Furthermore, we summarize current knowledge of the impact of COVID-19 on mental health of the populations of Western countries such as the United States, the United Kingdom, and Italy. Moreover, we discuss the influence of racial disparities in delivery of healthcare in the United States and their effects on the quality of, access to, and awareness of mental health care. Our awareness of these issues has the potential to inform further research, aid, and funding to the populations where it is most needed. Finally, we make recommendations for the direction of further research based on the findings of this article.
Racial disparities in opioid use disorder and its treatment: A review and commentary on the literature
Sean Lynch 1,2 , Faris Katkhuda 2,3 , Lidia Klepacz 2,4 , Eldene Towey 2,4 , Stephen J. Ferrando 2,4* 1 Department of Psychiatry, Icahn School of Medicine at Mount Sinai, Mount Sinai Beth Israel, NY, USA 2 Department of Psychiatry and Behavioral Sciences, New York Medical College, School of Medicine, NY, USA 3 Department of Psychiatry, Boston Medical Center, Massachusetts, USA 4 Department of Psychiatry, Westchester Medical Center Health Network, Behavioral Health Center, NY, USA
Despite public interventions, the rate of opioid use disorder (OUD) continues to rise. In this focused review of the existing literature, the authors describe how increases in OUD, as well as opioid-related deaths, have occurred disproportionately among people of color. Black patients in particular are dying of overdose at an increased rate, however are less likely to receive any treatment for OUD. Additionally, Black patients are less likely to receive buprenorphine than White patients, but more likely to receive methadone. Potential causes of these disparities are discussed, as well as the impact of the COVID-19 pandemic, and the successes of several pilot programs.
Longitudinal trajectories of region-level suicide mortality in Tokyo, Japan, 2011 to 2021
Asuka Suzuki 1 , Kazue Yamaoka 1 *, Mariko Inoue 1 , Toshiro Tango 2,1 1 Teikyo University Graduate School of Public Health, Tokyo, Japan 2 Center for Medical Statistics, Tokyo, Japan
Background: Suicide mortality in Japan has declined over a period of more than 10 years, however, differences in longitudinal trajectories at a regional level are not well characterized. Objective was to clarify the longitudinal suicide mortality trajectories at the regional level in Tokyo from 2011 to 2021 by considering spatial smoothing, before and during the COVID-19 pandemic.
Methods : This longitudinal cross-sectional analysis used fifty-four regions in Tokyo, Japan. Suicide mortality trends used data from the Cabinet Office of the Japanese government from 2011 to 2021. Regional social and environmental characteristics were used as 10 covariates. Empirical Bayes estimates for the standardized mortality ratio were obtained. A conditional autoregressive (CAR) model was applied to capture the spatial correlation for a crude and adjusted with 10 covariates using OpenBUGS. Spatial clusters were also identified by FlexScan, SaTScan, and Tango’s test.
Results: Longitudinal trajectories for both males and females were similar to a decreasing trend in all Japan until 2019. In 2020, the beginning of the COVID-19 pandemic, the age-specific suicide deaths were the highest among those in their 20s. However, those were the highest among males in their 50s in 2021. The results of the CAR models adjusted for 10 covariates detected several regions as having higher suicide rates, but those regions were somewhat varied.
Conclusion: During the COVID-19 pandemic, both sexes in their 20s and males in their 50s showed a tendency toward an increase in suicides. The detected regions by spatial epidemiology varied with sex.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Mental Health Prevention and Promotion—A Narrative Review
Vijender singh, akash kumar, snehil gupta.
- Author information
- Article notes
- Copyright and License information
Edited by: Samrat Singh Bhandari, Sikkim Manipal University, India
Reviewed by: Seshadri Sekhar Chatterjee, West Bengal University of Health Sciences, India; Arabinda Brahma, Girindra Sekhar Clinic Kolkata, India; Olusegun Baiyewu, University of Ibadan, Nigeria
*Correspondence: Snehil Gupta [email protected]
This article was submitted to Public Mental Health, a section of the journal Frontiers in Psychiatry
Received 2022 Mar 16; Accepted 2022 Jun 8; Collection date 2022.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Extant literature has established the effectiveness of various mental health promotion and prevention strategies, including novel interventions. However, comprehensive literature encompassing all these aspects and challenges and opportunities in implementing such interventions in different settings is still lacking. Therefore, in the current review, we aimed to synthesize existing literature on various mental health promotion and prevention interventions and their effectiveness. Additionally, we intend to highlight various novel approaches to mental health care and their implications across different resource settings and provide future directions. The review highlights the (1) concept of preventive psychiatry, including various mental health promotions and prevention approaches, (2) current level of evidence of various mental health preventive interventions, including the novel interventions, and (3) challenges and opportunities in implementing concepts of preventive psychiatry and related interventions across the settings. Although preventive psychiatry is a well-known concept, it is a poorly utilized public health strategy to address the population's mental health needs. It has wide-ranging implications for the wellbeing of society and individuals, including those suffering from chronic medical problems. The researchers and policymakers are increasingly realizing the potential of preventive psychiatry; however, its implementation is poor in low-resource settings. Utilizing novel interventions, such as mobile-and-internet-based interventions and blended and stepped-care models of care can address the vast mental health need of the population. Additionally, it provides mental health services in a less-stigmatizing and easily accessible, and flexible manner. Furthermore, employing decision support systems/algorithms for patient management and personalized care and utilizing the digital platform for the non-specialists' training in mental health care are valuable additions to the existing mental health support system. However, more research concerning this is required worldwide, especially in the low-and-middle-income countries.
Keywords: mental health, promotion, prevention, protection, intervention, review, preventive psychiatry, novel interventions
Introduction
Mental disorder has been recognized as a significant public health concern and one of the leading causes of disability worldwide, particularly with the loss of productive years of the sufferer's life ( 1 ). The Global Burden of Disease report (2019) highlights an increase, from around 80 million to over 125 million, in the worldwide number of Disability-Adjusted Life Years (DALYs) attributable to mental disorders. With this surge, mental disorders have moved into the top 10 significant causes of DALYs worldwide over the last three decades ( 2 ). Furthermore, this data does not include substance use disorders (SUDs), which, if included, would increase the estimated burden manifolds. Moreover, if the caregiver-related burden is accounted for, this figure would be much higher. Individual, social, cultural, political, and economic issues are critical mental wellbeing determinants. An increasing burden of mental diseases can, in turn, contribute to deterioration in physical health and poorer social and economic growth of a country ( 3 ). Mental health expenditure is roughly 3–4% of their Gross Domestic Products (GDPs) in developed regions of the world; however, the figure is abysmally low in low-and-middle-income countries (LMICs) ( 4 ). Untreated mental health and behavioral problems in childhood and adolescents, in particular, have profound long-term social and economic adverse consequences, including increased contact with the criminal justice system, lower employment rate and lesser wages among those employed, and interpersonal difficulties ( 5 – 8 ).
Need for Mental Health (MH) Prevention
Longitudinal studies suggest that individuals with a lower level of positive wellbeing are more likely to acquire mental illness ( 9 ). Conversely, factors that promote positive wellbeing and resilience among individuals are critical in preventing mental illnesses and better outcomes among those with mental illness ( 10 , 11 ). For example, in patients with depressive disorders, higher premorbid resilience is associated with earlier responses ( 12 ). On the contrary, patients with bipolar affective- and recurrent depressive disorders who have a lower premorbid quality of life are at higher risk of relapses ( 13 ).
Recently there has been an increased emphasis on the need to promote wellbeing and positive mental health in preventing the development of mental disorders, for poor mental health has significant social and economic implications ( 14 – 16 ). Research also suggests that mental health promotion and preventative measures are cost-effective in preventing or reducing mental illness-related morbidity, both at the society and individual level ( 17 ).
Although the World Health Organization (WHO) defines health as “a state of complete physical, mental, and social wellbeing and not merely an absence of disease or infirmity,” there has been little effort at the global level or stagnation in implementing effective mental health services ( 18 ). Moreover, when it comes to the research on mental health (vis-a-viz physical health), promotive and preventive mental health aspects have received less attention vis-a-viz physical health. Instead, greater emphasis has been given to the illness aspect, such as research on psychopathology, mental disorders, and treatment ( 19 , 20 ). Often, physicians and psychiatrists are unfamiliar with various concepts, approaches, and interventions directed toward mental health promotion and prevention ( 11 , 21 ).
Prevention and promotion of mental health are essential, notably in reducing the growing magnitude of mental illnesses. However, while health promotion and disease prevention are universally regarded concepts in public health, their strategic application for mental health promotion and prevention are often elusive. Furthermore, given the evidence of substantial links between psychological and physical health, the non-incorporation of preventive mental health services is deplorable and has serious ramifications. Therefore, policymakers and health practitioners must be sensitized about linkages between mental- and physical health to effectively implement various mental health promotive and preventive interventions, including in individuals with chronic physical illnesses ( 18 ).
The magnitude of the mental health problems can be gauged by the fact that about 10–20% of young individuals worldwide experience depression ( 22 ). As described above, poor mental health during childhood is associated with adverse health (e.g., substance use and abuse), social (e.g., delinquency), academic (e.g., school failure), and economic (high risk of poverty) adverse outcomes in adulthood ( 23 ). Childhood and adolescence are critical periods for setting the ground for physical growth and mental wellbeing ( 22 ). Therefore, interventions promoting positive psychology empower youth with the life skills and opportunities to reach their full potential and cope with life's challenges. Comprehensive mental health interventions involving families, schools, and communities have resulted in positive physical and psychological health outcomes. However, the data is limited to high-income countries (HICs) ( 24 – 28 ).
In contrast, in low and middle-income countries (LMICs) that bear the greatest brunt of mental health problems, including massive, coupled with a high treatment gap, such interventions remained neglected in public health ( 29 , 30 ). This issue warrants prompt attention, particularly when global development strategies such as Millennium Development Goals (MDGs) realize the importance of mental health ( 31 ). Furthermore, studies have consistently reported that people with socioeconomic disadvantages are at a higher risk of mental illness and associated adverse outcomes; partly, it is attributed to the inequitable distribution of mental health services ( 32 – 35 ).
Scope of Mental Health Promotion and Prevention in the Current Situation
Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses ( 18 , 36 – 42 ). There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe mental diseases (e.g., schizophrenia and psychotic illness, and bipolar affective disorders) as well as common mental disorders (e.g., anxiety, depression, stress-related disorders) ( 43 – 46 ). These preventive measures have also been evaluated for their cost-effectiveness with promising findings. In addition, novel interventions such as digital-based interventions and novel therapies (e.g., adventure therapy, community pharmacy program, and Home-based Nurse family partnership program) to address the mental health problems have yielded positive results. Likewise, data is emerging from LMICs, showing at least moderate evidence of mental health promotion intervention effectiveness. However, most of the available literature and intervention is restricted mainly to the HICs ( 47 ). Therefore, their replicability in LMICs needs to be established and, also, there is a need to develop locally suited interventions.
Fortunately, there has been considerable progress in preventive psychiatry over recent decades, including research on it. In the light of these advances, there is an accelerated interest among researchers, clinicians, governments, and policymakers to harness the potentialities of the preventive strategies to improve the availability, accessibility, and utility of such services for the community.
The Concept of Preventive Psychiatry
Origins of preventive psychiatry.
The history of preventive psychiatry can be traced back to the early 1900's with the foundation of the national mental health association (erstwhile mental health association), the committee on mental hygiene in New York, and the mental health hygiene movement ( 48 ). The latter emphasized the need for physicians to develop empathy and recognize and treat mental illness early, leading to greater awareness about mental health prevention ( 49 ). Despite that, preventive psychiatry remained an alien concept for many, including mental health professionals, particularly when the etiology of most psychiatric disorders was either unknown or poorly understood. However, recent advances in our understanding of the phenomena underlying psychiatric disorders and availability of the neuroimaging and electrophysiological techniques concerning mental illness and its prognosis has again brought the preventive psychiatry in the forefront ( 1 ).
Levels of Prevention
The literal meaning of “prevention” is “the act of preventing something from happening” ( 50 ); the entity being prevented can range from the risk factors of the development of the illness, the onset of illness, or the recurrence of the illness or associated disability. The concept of prevention emerged primarily from infectious diseases; measures like mass vaccination and sanitation promotion have helped prevent the development of the diseases and subsequent fatalities. The original preventive model proposed by the Commission on Chronic Illness in 1957 included primary, secondary, and tertiary preventions ( 48 ).

The Concept of Primary, Secondary, and Tertiary Prevention
The stages of prevention target distinct aspects of the illness's natural course; the primary prevention acts at the stage of pre-pathogenesis, that is, when the disease is yet to occur, whereas the secondary and tertiary prevention target the phase after the onset of the disease ( 51 ). Primary prevention includes health promotion and specific protection, while secondary and tertairy preventions include early diagnosis and treatment and measures to decrease disability and rehabilitation, respectively ( 51 ) ( Figure 1 ).
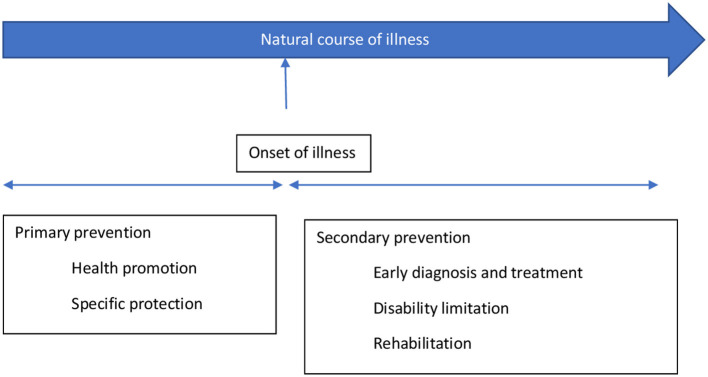
The concept of primary and secondary prevention [adopted from prevention: Primary, Secondary, Tertiary by Bauman et al. ( 51 )].
The primary prevention targets those individuals vulnerable to developing mental disorders and their consequences because of their bio-psycho-social attributes. Therefore, it can be viewed as an intervention to prevent an illness, thereby preventing mental health morbidity and potential social and economic adversities. The preventive strategies under it usually target the general population or individuals at risk. Secondary and tertiary prevention targets those who have already developed the illness, aiming to reduce impairment and morbidity as soon as possible. However, these measures usually occur in a person who has already developed an illness, therefore facing related suffering, hence may not always be successful in curing or managing the illness. Thus, secondary and tertiary prevention measures target the already exposed or diagnosed individuals.
The Concept of Universal, Selective, and Indicated Prevention
The classification of health prevention based on primary/secondary/tertiary prevention is limited in being highly centered on the etiology of the illness; it does not consider the interaction between underlying etiology and risk factors of an illness. Gordon proposed another model of prevention that focuses on the degree of risk an individual is at, and accordingly, the intensity of intervention is determined. He has classified it into universal, selective, and indicated prevention. A universal preventive strategy targets the whole population irrespective of individual risk (e.g., maintaining healthy, psychoactive substance-free lifestyles); selective prevention is targeted to those at a higher risk than the general population (socio-economically disadvantaged population, e.g., migrants, a victim of a disaster, destitute, etc.). The indicated prevention aims at those who have established risk factors and are at a high risk of getting the disease (e.g., family history of psychiatric illness, history of substance use, certain personality types, etc.). Nevertheless, on the other hand, these two classifications (the primary, secondary, and tertiary prevention; and universal, selective, and indicated prevention) have been intended for and are more appropriate for physical illnesses with a clear etiology or risk factors ( 48 ).
In 1994, the Institute of Medicine (IOM) Committee on Prevention of Mental Disorders proposed a new paradigm that classified primary preventive measures for mental illnesses into three categories. These are indicated, selected, and universal preventive interventions (refer Figure 2 ). According to this paradigm, primary prevention was limited to interventions done before the onset of the mental illness ( 48 ). In contrast, secondary and tertiary prevention encompasses treatment and maintenance measures ( Figure 2 ).
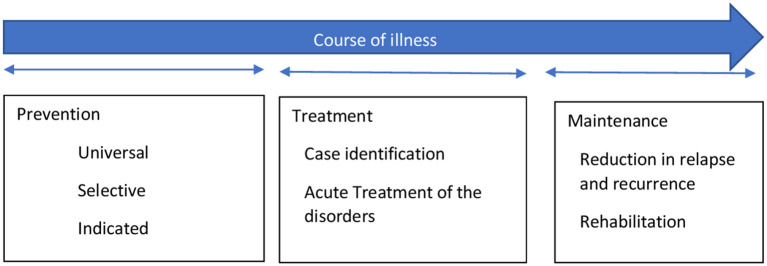
The interventions for mental illness as classified by the Institute of Medicine (IOM) Committee on Prevention of Mental Disorders [adopted from Mrazek and Haggerty ( 48 )].
Although the boundaries between prevention and treatment are often more overlapping than being exclusive, the new paradigm can be used to avoid confusion stemming from the common belief that prevention can take place at all parts of mental health management ( 48 ). The onset of mental illnesses can be prevented by risk reduction interventions, which can involve reducing risk factors in an individual and strengthening protective elements in them. It aims to target modifiable factors, both risk, and protective factors, associated with the development of the illness through various general and specific interventions. These interventions can work across the lifespan. The benefits are not restricted to reduction or delay in the onset of illness but also in terms of severity or duration of illness ( 48 ).On the spectrum of mental health interventions, universal preventive interventions are directed at the whole population without identifiable risk factors. The interventions are beneficial for the general population or sub-groups. Prenatal care and childhood vaccination are examples of preventative measures that have benefited both physical and mental health. Selective preventive mental health interventions are directed at people or a subgroup with a significantly higher risk of developing mental disorders than the general population. Risk groups are those who, because of their vulnerabilities, are at higher risk of developing mental illnesses, e.g., infants with low-birth-weight (LBW), vulnerable children with learning difficulties or victims of maltreatment, elderlies, etc. Specific interventions are home visits and new-born day care facilities for LBW infants, preschool programs for all children living in resource-deprived areas, support groups for vulnerable elderlies, etc. Indicated preventive interventions focus on high-risk individuals who have developed minor but observable signs or symptoms of mental disorder or genetic risk factors for mental illness. However, they have not fulfilled the criteria of a diagnosable mental disorder. For instance, the parent-child interaction training program is an indicated prevention strategy that offers support to children whose parents have recognized them as having behavioral difficulties.
The overall objective of mental health promotion and prevention is to reduce the incidence of new cases, additionally delaying the emergence of mental illness. However, promotion and prevention in mental health complement each other rather than being mutually exclusive. Moreover, combining these two within the overall public health framework reduces stigma, increases cost-effectiveness, and provides multiple positive outcomes ( 18 ).
How Prevention in Psychiatry Differs From Other Medical Disorders
Compared to physical illnesses, diagnosing a mental illness is more challenging, particularly when there is still a lack of objective assessment methods, including diagnostic tools and biomarkers. Therefore, the diagnosis of mental disorders is heavily influenced by the assessors' theoretical perspectives and subjectivity. Moreover, mental illnesses can still be considered despite an individual not fulfilling the proper diagnostic criteria led down in classificatory systems, but there is detectable dysfunction. Furthermore, the precise timing of disorder initiation or transition from subclinical to clinical condition is often uncertain and inconclusive ( 48 ). Therefore, prevention strategies are well-delineated and clear in the case of physical disorders while it's still less prevalent in mental health parlance.
Terms, Definitions, and Concepts
The terms mental health, health promotion, and prevention have been differently defined and interpreted. It is further complicated by overlapping boundaries of the concept of promotion and prevention. Some commonly used terms in mental health prevention have been tabulated ( Table 1 ) ( 18 ).
Commonly used terms in mental health prevention.
Mental Health Promotion and Protection
The term “mental health promotion” also has definitional challenges as it signifies different things to different individuals. For some, it means the treatment of mental illness; for others, it means preventing the occurrence of mental illness; while for others, it means increasing the ability to manage frustration, stress, and difficulties by strengthening one's resilience and coping abilities ( 54 ). It involves promoting the value of mental health and improving the coping capacities of individuals rather than amelioration of symptoms and deficits.
Mental health promotion is a broad concept that encompasses the entire population, and it advocates for a strengths-based approach and tries to address the broader determinants of mental health. The objective is to eliminate health inequalities via empowerment, collaboration, and participation. There is mounting evidence that mental health promotion interventions improve mental health, lower the risk of developing mental disorders ( 48 , 55 , 56 ) and have socioeconomic benefits ( 24 ). In addition, it strives to increase an individual's capacity for psychosocial wellbeing and adversity adaptation ( 11 ).
However, the concepts of mental health promotion, protection, and prevention are intrinsically linked and intertwined. Furthermore, most mental diseases result from complex interaction risk and protective factors instead of a definite etiology. Facilitating the development and timely attainment of developmental milestones across an individual's lifespan is critical for positive mental health ( 57 ). Although mental health promotion and prevention are essential aspects of public health with wide-ranging benefits, their feasibility and implementation are marred by financial and resource constraints. The lack of cost-effectiveness studies, particularly from the LMICs, further restricts its full realization ( 47 , 58 , 59 ).
Despite the significance of the topic and a considerable amount of literature on it, a comprehensive review is still lacking that would cover the concept of mental health promotion and prevention and simultaneously discusses various interventions, including the novel techniques delivered across the lifespan, in different settings, and level of prevention. Therefore, this review aims to analyze the existing literature on various mental health promotion and prevention-based interventions and their effectiveness. Furthermore, its attempts to highlight the implications of such intervention in low-resource settings and provides future directions. Such literature would add to the existing literature on mental health promotion and prevention research and provide key insights into the effectiveness of such interventions and their feasibility and replicability in various settings.
Methodology
For the current review, key terms like “mental health promotion,” OR “protection,” OR “prevention,” OR “mitigation” were used to search relevant literature on Google Scholar, PubMed, and Cochrane library databases, considering a time period between 2000 to 2019 ( Supplementary Material 1 ). However, we have restricted our search till 2019 for non-original articles (reviews, commentaries, viewpoints, etc.), assuming that it would also cover most of the original articles published until then. Additionally, we included original papers from the last 5 years (2016–2021) so that they do not get missed out if not covered under any published review. The time restriction of 2019 for non-original articles was applied to exclude papers published during the Coronavirus disease (COVID-19) pandemic as the latter was a significant event, bringing about substantial change and hence, it warranted a different approach to cater to the MH needs of the population, including MH prevention measures. Moreover, the COVID-19 pandemic resulted in the flooding of novel interventions for mental health prevention and promotion, specifically targeting the pandemic and its consequences, which, if included, could have biased the findings of the current review on various MH promotion and prevention interventions.
A time frame of about 20 years was taken to see the effectiveness of various MH promotion and protection interventions as it would take substantial time to be appreciated in real-world situations. Therefore, the current paper has put greater reliance on the review articles published during the last two decades, assuming that it would cover most of the original articles published until then.
The above search yielded 320 records: 225 articles from Google scholar, 59 articles from PubMed, and 36 articles from the Cochrane database flow-diagram of records screening. All the records were title/abstract screened by all the authors to establish the suitability of those records for the current review; a bibliographic- and gray literature search was also performed. In case of any doubts or differences in opinion, it was resolved by mutual discussion. Only those articles directly related to mental health promotion, primary prevention, and related interventions were included in the current review. In contrast, records that discussed any specific conditions/disorders (post-traumatic stress disorders, suicide, depression, etc.), specific intervention (e.g., specific suicide prevention intervention) that too for a particular population (e.g., disaster victims) lack generalizability in terms of mental health promotion or prevention, those not available in the English language, and whose full text was unavailable were excluded. The findings of the review were described narratively.
Interventions for Mental Health Promotion and Prevention and Their Evidence
Various interventions have been designed for mental health promotion and prevention. They are delivered and evaluated across the regions (high-income countries to low-resource settings, including disaster-affiliated regions of the world), settings (community-based, school-based, family-based, or individualized); utilized different psychological constructs and therapies (cognitive behavioral therapy, behavioral interventions, coping skills training, interpersonal therapies, general health education, etc.); and delivered by different professionals/facilitators (school-teachers, mental health professionals or paraprofessionals, peers, etc.). The details of the studies, interventions used, and outcomes have been provided in Supplementary Table 1 . Below we provide the synthesized findings of the available research.
The majority of the available studies were quantitative and experimental. Randomized controlled trials comprised a sizeable proportion of the studies; others were quasi-experimental studies and, a few, qualitative studies. The studies primarily focussed on school students or the younger population, while others were explicitly concerned with the mental health of young females ( 60 ). Newer data is emerging on mental health promotion and prevention interventions for elderlies (e.g., dementia) ( 61 ). The majority of the research had taken a broad approach to mental health promotion ( 62 ). However, some studies have focused on universal prevention ( 63 , 64 ) or selective prevention ( 65 – 68 ). For instance, the Resourceful Adolescent Program (RAPA) was implemented across the schools and has utilized cognitive-behavioral and interpersonal therapies and reported a significant improvement in depressive symptoms. Some of the interventions were directed at enhancing an individual's characteristics like resilience, behavior regulation, and coping skills (ZIPPY's Friends) ( 69 ), while others have focused on the promotion of social and emotional competencies among the school children and attempted to reduce the gap in such competencies across the socio-economic classes (“Up” program) ( 70 ) or utilized expressive abilities of the war-affected children (Writing for Recover (WfR) intervention) ( 71 ) to bring about an improvement in their psychological problems (a type of selective prevention) ( 62 ) or harnessing the potential of Art, in the community-based intervention, to improve self-efficacy, thus preventing mental disorders (MAD about Art program) ( 72 ). Yet, others have focused on strengthening family ( 60 , 73 ), community relationships ( 62 ), and targeting modifiable risk factors across the life course to prevent dementia among the elderlies and also to support the carers of such patients ( 61 ).
Furthermore, more of the studies were conducted and evaluated in the developed parts of the world, while emerging economies, as anticipated, far lagged in such interventions or related research. The interventions that are specifically adapted for local resources, such as school-based programs involving paraprofessionals and teachers in the delivery of mental health interventions, were shown to be more effective ( 62 , 74 ). Likewise, tailored approaches for low-resource settings such as LMICs may also be more effective ( 63 ). Some of these studies also highlight the beneficial role of a multi-dimensional approach ( 68 , 75 ) and interventions targeting early lifespan ( 76 , 77 ).
Newer Insights: How to Harness Digital Technology and Novel Methods of MH Promotion and Protection
With the advent of digital technology and simultaneous traction on mental health promotion and prevention interventions, preventive psychiatrists and public health experts have developed novel techniques to deliver mental health promotive and preventive interventions. These encompass different settings (e.g., school, home, workplace, the community at large, etc.) and levels of prevention (universal, selective, indicated) ( 78 – 80 ).
The advanced technologies and novel interventions have broadened the scope of MH promotion and prevention, such as addressing the mental health issues of individuals with chronic medical illness ( 81 , 82 ), severe mental disorders ( 83 ), children and adolescents with mental health problems, and geriatric population ( 78 ). Further, it has increased the accessibility and acceptability of such interventions in a non-stigmatizing and tailored manner. Moreover, they can be integrated into the routine life of the individuals.
For instance, Internet-and Mobile-based interventions (IMIs) have been utilized to monitor health behavior as a form of MH prevention and a stand-alone self-help intervention. Moreover, the blended approach has expanded the scope of MH promotive and preventive interventions such as face-to-face interventions coupled with remote therapies. Simultaneously, it has given way to the stepped-care (step down or step-up care) approach of treatment and its continuation ( 79 ). Also, being more interactive and engaging is particularly useful for the youth.
The blended model of care has utilized IMIs to a varying degree and at various stages of the psychological interventions. This includes IMIs as a supplementary approach to the face-to-face-interventions (FTFI), FTFI augmented by behavior intervention technologies (BITs), BITs augmented by remote human support, and fully automated BITs ( 84 ).
The stepped care model of mental health promotion and prevention strategies includes a stepped-up approach, wherein BITs are utilized to manage the prodromal symptoms, thereby preventing the onset of the full-blown episode. In the Stepped-down approach, the more intensive treatments (in-patient or out-patient based interventions) are followed and supplemented with the BITs to prevent relapse of the mental illness, such as for previously admitted patients with depression or substance use disorders ( 85 , 86 ).
Similarly, the latest research has developed newer interventions for strengthening the psychological resilience of the public or at-risk individuals, which can be delivered at the level of the home, such as, e.g., nurse family partnership program (to provide support to the young and vulnerable mothers and prevent childhood maltreatment) ( 87 ); family healing together program aimed at improving the mental health of the family members living with persons with mental illness (PwMI) ( 88 ). In addition, various novel interventions for MH promotion and prevention have been highlighted in the Table 2 .
Depiction of various novel mental health promotion and prevention strategies.
MH stigma, understanding MH and wellness, information about different mental disorders, experiences of mental illnesses, help seeking and garnering support, and importance of positive MH .
a/w, associated with; A-V, audio-visual; b/w, between; CBT, Cognitive Behavioral Therapy; CES-Dep., Center for Epidemiologic Studies-Depression scale; CG, control group; FU, follow-up; GAD, generalized anxiety disorders-7; IA, intervention arm; HCWs, Health Care Workers; LMIC, low and middle-income countries; MDD, major depressive disorders; mgt, management; MH, mental health; MHP, mental health professional; MINI, mini neuropsychiatric interview; NNT, number needed to treat; PHQ-9, patient health questionnaire; TAU, treatment as usual .
Furthermore, school/educational institutes-based interventions such as school-Mental Health Magazines to increase mental health literacy among the teachers and students have been developed ( 80 ). In addition, workplace mental health promotional activities have targeted the administrators, e.g., guided “e-learning” for the managers that have shown to decrease the mental health problems of the employees ( 102 ).
Likewise, digital technologies have also been harnessed in strengthening community mental health promotive/preventive services, such as the mental health first aid (MHFA) Books on Prescription initiative in New Zealand provided information and self-help tools through library networks and trained book “prescribers,” particularly in rural and remote areas ( 103 ).
Apart from the common mental disorders such as depression, anxiety, and behavioral disorders in the childhood/adolescents, novel interventions have been utilized to prevent the development of or management of medical, including preventing premature mortality and psychological issues among the individuals with severe mental illnesses (SMIs), e.g., Lets' talk about tobacco-web based intervention and motivational interviewing to prevent tobacco use, weight reduction measures, and promotion of healthy lifestyles (exercise, sleep, and balanced diets) through individualized devices, thereby reducing the risk of cardiovascular disorders ( 83 ). Similarly, efforts have been made to improve such individuals' coping skills and employment chances through the WorkingWell mobile application in the US ( 104 ).
Apart from the digital-based interventions, newer, non-digital-based interventions have also been utilized to promote mental health and prevent mental disorders among individuals with chronic medical conditions. One such approach in adventure therapy aims to support and strengthen the multi-dimensional aspects of self. It includes the physical, emotional or cognitive, social, spiritual, psychological, or developmental rehabilitation of the children and adolescents with cancer. Moreover, it is delivered in the natural environment outside the hospital premises, shifting the focus from the illness model to the wellness model ( 81 ). Another strength of this intervention is it can be delivered by the nurses and facilitate peer support and teamwork.
Another novel approach to MH prevention is gut-microbiota and dietary interventions. Such interventions have been explored with promising results for the early developmental disorders (Attention deficit hyperactive disorder, Autism spectrum disorders, etc.) ( 105 ). It works under the framework of the shared vulnerability model for common mental disorders and other non-communicable diseases and harnesses the neuroplasticity potential of the developing brain. Dietary and lifestyle modifications have been recommended for major depressive disorders by the Clinical Practice Guidelines in Australia ( 106 ). As most childhood mental and physical disorders are determined at the level of the in-utero and early after the birth period, targeting maternal nutrition is another vital strategy. The utility has been expanded from maternal nutrition to women of childbearing age. The various novel mental health promotion and prevention strategies are shown in Table 2 .
Newer research is emerging that has utilized the digital platform for training non-specialists in diagnosis and managing individuals with mental health problems, such as Atmiyata Intervention and The SMART MH Project in India, and The Allillanchu Project in Peru, to name a few ( 99 ). Such frameworks facilitate task-sharing by the non-specialist and help in reducing the treatment gap in these countries. Likewise, digital algorithms or decision support systems have been developed to make mental health services more transparent, personalized, outcome-driven, collaborative, and integrative; one such example is DocuMental, a clinical decision support system (DSS). Similarly, frameworks like i-PROACH, a cloud-based intelligent platform for research outcome assessment and care in mental health, have expanded the scope of the mental health support system, including promoting research in mental health ( 100 ). In addition, COVID-19 pandemic has resulted in wider dissemination of the applications based on the evidence-based psycho-social interventions such as National Health Service's (NHS's) Mind app and Headspace (teaching meditation via a website or a phone application) that have utilized mindfulness-based practices to address the psychological problems of the population ( 101 ).
Challenges in Implementing Novel MH Promotion and Prevention Strategies
Although novel interventions, particularly internet and mobile-based interventions (IMIs), are effective models for MH promotion and prevention, their cost-effectiveness requires further exploration. Moreover, their feasibility and acceptability in LMICs could be challenging. Some of these could be attributed to poor digital literacy, digital/network-related limitations, privacy issues, and society's preparedness to implement these interventions.
These interventions need to be customized and adapted according to local needs and context, for which implementation and evaluative research are warranted. In addition, the infusion of more human and financial resources for such activities is required. Some reports highlight that many of these interventions do not align with the preferences and use the pattern of the service utilizers. For instance, one explorative research on mental health app-based interventions targeting youth found that despite the burgeoning applications, they are not aligned with the youth's media preferences and learning patterns. They are less interactive, have fewer audio-visual displays, are not youth-specific, are less dynamic, and are a single touch app ( 107 ).
Furthermore, such novel interventions usually come with high costs. In low-resource settings where service utilizers have limited finances, their willingness to use such services may be doubtful. Moreover, insurance companies, including those in high-income countries (HICs), may not be willing to fund such novel interventions, which restricts the accessibility and availability of interventions.
Research points to the feasibility and effectiveness of incorporating such novel interventions in routine services such as school, community, primary care, or settings, e.g., in low-resource settings, the resource persons like teachers, community health workers, and primary care physicians are already overburdened. Therefore, their willingness to take up additional tasks may raise skepticism. Moreover, the attitudinal barrier to moving from the traditional service delivery model to the novel methods may also impede.
Considering the low MH budget and less priority on the MH prevention and promotion activities in most low-resource settings, the uptake of such interventions in the public health framework may be lesser despite the latter's proven high cost-effectiveness. In contrast, policymakers may be more inclined to invest in the therapeutic aspects of MH.
Such interventions open avenues for personalized and precision medicine/health care vs. the traditional model of MH promotion and preventive interventions ( 108 , 109 ). For instance, multivariate prediction algorithms with methods of machine learning and incorporating biological research, such as genetics, may help in devising tailored, particularly for selected and indicated prevention, interventions for depression, suicide, relapse prevention, etc. ( 79 ). Therefore, more research in this area is warranted.
To be more clinically relevant, greater biological research in MH prevention is required to identify those at higher risk of developing given mental disorders due to the existing risk factors/prominent stress ( 110 ). For instance, researchers have utilized the transcriptional approach to identify a biological fingerprint for susceptibility (denoting abnormal early stress response) to develop post-traumatic stress disorders among the psychological trauma survivors by analyzing the expression of the Peripheral blood mononuclear cell gene expression profiles ( 111 ). Identifying such biological markers would help target at-risk individuals through tailored and intensive interventions as a form of selected prevention.
Similarly, such novel interventions can help in targeting the underlying risk such as substance use, poor stress management, family history, personality traits, etc. and protective factors, e.g., positive coping techniques, social support, resilience, etc., that influences the given MH outcome ( 79 ). Therefore, again, it opens the scope of tailored interventions rather than a one-size-fits-all model of selective and indicated prevention for various MH conditions.
Furthermore, such interventions can be more accessible for the hard-to-reach populations and those with significant mental health stigma. Finally, they play a huge role in ensuring the continuity of care, particularly when community-based MH services are either limited or not available. For instance, IMIs can maintain the improvement of symptoms among individuals previously managed in-patient, such as for suicide, SUDs, etc., or receive intensive treatment like cognitive behavior therapy (CBT) for depression or anxiety, thereby helping relapse prevention ( 86 , 112 ). Hence, such modules need to be developed and tested in low-resource settings.
IMIs (and other novel interventions) being less stigmatizing and easily accessible, provide a platform to engage individuals with chronic medical problems, e.g., epilepsy, cancer, cardiovascular diseases, etc., and non-mental health professionals, thereby making it more relevant and appealing for them.
Lastly, research on prevention-interventions needs to be more robust to adjust for the pre-intervention matching, high attrition rate, studying the characteristics of treatment completers vs. dropouts, and utilizing the intention-to-treat analysis to gauge the effect of such novel interventions ( 78 ).
Recommendations for Low-and-Middle-Income Countries
Although there is growing research on the effectiveness and utility of mental health promotion/prevention interventions across the lifespan and settings, low-resource settings suffer from specific limitations that restrict the full realization of such public health strategies, including implementing the novel intervention. To overcome these challenges, some of the potential solutions/recommendations are as follows:
The mental health literacy of the population should be enhanced through information, education, and communication (IEC) activities. In addition, these activities should reduce stigma related to mental problems, early identification, and help-seeking for mental health-related issues.
Involving teachers, workplace managers, community leaders, non-mental health professionals, and allied health staff in mental health promotion and prevention is crucial.
Mental health concepts and related promotion and prevention should be incorporated into the education curriculum, particularly at the medical undergraduate level.
Training non-specialists such as community health workers on mental health-related issues across an individual's life course and intervening would be an effective strategy.
Collaborating with specialists from other disciplines, including complementary and alternative medicines, would be crucial. A provision of an integrated health system would help in increasing awareness, early identification, and prompt intervention for at-risk individuals.
Low-resource settings need to develop mental health promotion interventions such as community-and school-based interventions, as these would be more culturally relevant, acceptable, and scalable.
Utilizing a digital platform for scaling mental health services (e.g., telepsychiatry services to at-risk populations) and training the key individuals in the community would be a cost-effective framework that must be explored.
Infusion of higher financial and human resources in this area would be a critical step, as, without adequate resources, research, service development, and implementation would be challenging.
It would also be helpful to identify vulnerable populations and intervene in them to prevent the development of clinical psychiatric disorders.
Lastly, involving individuals with lived experiences at the level of mental health planning, intervention development, and delivery would be cost-effective.
Clinicians, researchers, public health experts, and policymakers have increasingly realized mental health promotion and prevention. Investment in Preventive psychiatry appears to be essential considering the substantial burden of mental and neurological disorders and the significant treatment gap. Literature suggests that MH promotive and preventive interventions are feasible and effective across the lifespan and settings. Moreover, various novel interventions (e.g., internet-and mobile-based interventions, new therapies) have been developed worldwide and proven effective for mental health promotion and prevention; such interventions are limited mainly to HICs.
Despite the significance of preventive psychiatry in the current world and having a wide-ranging implication for the wellbeing of society and individuals, including those suffering from chronic medical problems, it is a poorly utilized public health field to address the population's mental health needs. Lately, researchers and policymakers have realized the untapped potentialities of preventive psychiatry. However, its implementation in low-resource settings is still in infancy and marred by several challenges. The utilization of novel interventions, such as digital-based interventions, and blended and stepped-care models of care, can address the enormous mental health need of the population. Additionally, it provides mental health services in a less-stigmatizing and easily accessible, and flexible manner. More research concerning this is required from the LMICs.
Author Contributions
VS, AK, and SG: methodology, literature search, manuscript preparation, and manuscript review. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.898009/full#supplementary-material
- 1. Trivedi JK, Tripathi A, Dhanasekaran S, Moussaoui D. Preventive psychiatry: concept appraisal and future directions. Int J Soc Psychiatry. (2014) 60:321–9. 10.1177/0020764013488570 [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Lond Engl. (2014) 384:766–81. 10.1016/S0140-6736(14)60460-8 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry Abingdon Engl. (2014) 26:392–407. 10.3109/09540261.2014.928270 [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Organization IL . Mental Health in the Workplace. Introduction. Geneva: International Labour Organization; (2000). Available online at: https://public.ebookcentral.proquest.com/choice/publicfullrecord.aspx?p=4954519 (accessed March 2, 2022). [ Google Scholar ]
- 5. Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. (2001) 323:191. 10.1136/bmj.323.7306.191 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Chen H, Cohen P, Kasen S, Johnson JG, Berenson K, Gordon K. Impact of adolescent mental disorders and physical illnesses on quality of life 17 years later. Arch Pediatr Adolesc Med. (2006) 160:93–9. 10.1001/archpedi.160.1.93 [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. McCrone P, Knapp M, Fombonne E. The Maudsley long-term follow-up of child and adolescent depression. Predicting costs in adulthood. Eur Child Adolesc Psychiatry. (2005) 14:407–13. 10.1007/s00787-005-0491-6 [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven: the consequences of conduct problems in childhood for psychosocial functioning in adulthood. J Child Psychol Psychiatry. (2005) 46:837–49. 10.1111/j.1469-7610.2004.00387.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Wood AM, Joseph S. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: a ten year cohort study. J Affect Disord. (2010) 122:213–7. 10.1016/j.jad.2009.06.032 [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Burton NW, Pakenham KI, Brown WJ. Feasibility and effectiveness of psychosocial resilience training: a pilot study of the READY program. Psychol Health Med. (2010) 15:266–77. 10.1080/13548501003758710 [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Kalra G, Christodoulou G, Jenkins R, Tsipas V, Christodoulou N, Lecic-Tosevski D, et al. Mental health promotion: guidance and strategies. Eur Psychiatry J Assoc Eur Psychiatr. (2012) 27:81–6. 10.1016/j.eurpsy.2011.10.001 [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Min JA, Lee NB, Lee CU, Lee C, Chae JH. Low trait anxiety, high resilience, and their interaction as possible predictors for treatment response in patients with depression. J Affect Disord. (2012) 137:61–9. 10.1016/j.jad.2011.12.026 [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Thunedborg K, Black CH, Bech P. Beyond the Hamilton depression scores in long-term treatment of manic-melancholic patients: prediction of recurrence of depression by quality of life measurements. Psychother Psychosom. (1995) 64:131–40. 10.1159/000289002 [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global Burden of Disease Risk Factors. Washington, DC: World Bank; (2006). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK11812/ (accessed February 28, 2022). [ Google Scholar ]
- 15. World Health Organization . WHO European Ministerial Conference on Mental Health (1st : 2005 : Helsinki F, World Health Organization. Regional Office for Europe. Mental health action plan for Europe : facing the challenges, building solutions. In: First WHO European Ministerial Conference on Mental Health, Helsinki, Finland. (EUR/04/5047810/7). (2005). Available from: https://apps.who.int/iris/handle/10665/107627 (accessed January 12–15, 2005).
- 16. Green Paper. Improving the Mental Health of the Population Towards a Strategy on Mental Health for the European Union. Brussels. p. 30. [ Google Scholar ]
- 17. Cuijpers P, Van Straten A, Smit F. Preventing the incidence of new cases of mental disorders: a meta-analytic review. J Nerv Ment Dis. (2005) 193:119–25. 10.1097/01.nmd.0000152810.76190.a6 [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Saxena S, Maulik PK, World Health Organization . Prevention and Promotion in Mental Health. Geneva: World Health Organization; (2002). [ Google Scholar ]
- 19. Herrman H. The need for mental health promotion. Aust N Z J Psychiatry. (2001) 35:709–15. 10.1046/j.1440-1614.2001.00947.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Ryff CD, Singer B. Psychological well-being: meaning, measurement, and implications for psychotherapy research. Psychother Psychosom. (1996) 65:14–23. 10.1159/000289026 [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Monshat K, Herrman H. What does “mental health promotion” mean to psychiatry trainees? Australas Psychiatry Bull R Aust N Z Coll Psychiatr. (2010) 18:589. 10.3109/10398562.2010.500330 [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet Lond Engl. (2011) 378:1515–25. 10.1016/S0140-6736(11)60827-1 [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Jenkins R, Baingana F, Ahmad R, McDaid D, Atun R. Social, economic, human rights and political challenges to global mental health. Ment Health Fam Med. (2011) 8:87–96. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Jané-Llopis E, Barry M, Hosman C, Patel V. Mental health promotion works: a review. Promot Educ. (2005) 12(Suppl.):9–25. 10.1177/10253823050120020103x [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Nores M, Barnett WS. Benefits of early childhood interventions across the world: (Under) Investing in the very young. Econ Educ Rev. (2010) 29:271–82. 10.1016/j.econedurev.2009.09.001 [ DOI ] [ Google Scholar ]
- 26. Baker-Henningham H, López Bóo F. Early Childhood Stimulation Interventions in Developing Countries: A Comprehensive Literature Review. Bonn: Institute for the Study of Labor. (2010). 10.2139/ssrn.1700451 Available online at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=1700451 [ DOI ] [ Google Scholar ]
- 27. Stewart-Brown SL, Schrader-McMillan A. Parenting for mental health: what does the evidence say we need to do? Report of Workpackage 2 of the DataPrev project. Health Promot Int. (2011) 26(Suppl.1):i10–28. 10.1093/heapro/dar056 [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Weare K, Nind M. Mental health promotion and problem prevention in schools: what does the evidence say? Health Promot Int. (2011) 26(Suppl.1):i29–69. 10.1093/heapro/dar075 [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Barry MM, Clarke AM, Jenkins R, Patel V. A systematic review of the effectiveness of mental health promotion interventions for young people in low and middle income countries. BMC Public Health. (2013) 13:1–19. 10.1186/1471-2458-13-835 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Patel V, Flisher AJ, Nikapota A, Malhotra S. Promoting child and adolescent mental health in low and middle income countries. J Child Psychol Psychiatry. (2008) 49:313–34. 10.1111/j.1469-7610.2007.01824.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Miranda JJ, Patel V. Achieving the millennium development goals: does mental health play a role? PLoS Med. (2005) 2:e291. 10.1371/journal.pmed.0020291 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. Fryers T, Melzer D, Jenkins R. Social inequalities and the common mental disorders: a systematic review of the evidence. Soc Psychiatry Psychiatr Epidemiol. (2003) 38:229–37. 10.1007/s00127-003-0627-2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Jenkins R, Bhugra D, Bebbington P, Brugha T, Farrell M, Coid J, et al. Debt, income and mental disorder in the general population. Psychol Med. (2008) 38:1485–93. 10.1017/S0033291707002516 [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med. (2010) 71:517–28. 10.1016/j.socscimed.2010.04.027 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. Blas E, Kurup AS. Equity, Social Determinants and Public Health Programmes. Available online at: https://apps.who.int/iris/handle/10665/44289 (accessed March 2, 2022).
- 36. Durlak JA, Wells AM. Primary prevention mental health programs: the future is exciting. Am J Community Psychol. (1997) 25:233–43. 10.1023/A:1024674631189 [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Durlak JA. Primary prevention mental health programs for children and adolescents are effective. J Ment Health. (1998) 7:463–9. 10.1080/0963823981784235101116 [ DOI ] [ Google Scholar ]
- 38. Lecic-Tosevski D, Christodoulou G, Herrman H, Hosman C, Jenkins R, Newton J, et al. WPA consensus statement on psychiatric prevention. Dyn Psychiatr Dyn Psychiatry. (2003) 36:307–19.8908416 [ Google Scholar ]
- 39. Kolbe LJ. Meta-analysis of interventions to prevent mental health problems among youth: a public health commentary. Am J Community Psychol. (1997) 25:227–32. 10.1023/A:1024622614351 [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Olds DL, Eckenrode J, Henderson CR, Kitzman H, Powers J, Cole R, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. J Am Med Assoc. (1997) 278:637–43. 10.1001/jama.1997.03550080047038 [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Andrews G, Wilkinson DD. The prevention of mental disorders in young people. Med J Aust. (2002) 177:S97–100. 10.5694/j.1326-5377.2002.tb04865.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. HEALTHEVIDENCE . The Prevention of Mental Disorders in School-Aged Children: Current State of the Field. Available online at: https://www.healthevidence.org/view-article.aspx?a=prevention-mental-disorders-school-aged-children-current-state-field-15455 (accessed March 2, 2022).
- 43. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev. (2011) 6:CD004718. 10.1002/14651858.CD004718.pub3 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Cuijpers P, van Straten A, Smits N, Smit F. Screening and early psychological intervention for depression in schools : systematic review and meta-analysis. Eur Child Adolesc Psychiatry. (2006) 15:300–7. 10.1007/s00787-006-0537-4 [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Neil AL, Christensen H. Australian school-based prevention and early intervention programs for anxiety and depression: a systematic review. Med J Aust. (2007) 186:305–8. 10.5694/j.1326-5377.2007.tb00906.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Merry S, McDowell H, Hetrick S, Bir J, Muller N. Psychological and/or educational interventions for the prevention of depression in children and adolescents. Cochrane Database Syst Rev. (2004) 1:CD003380. 10.1002/14651858.CD003380.pub2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Zechmeister I, Kilian R, McDaid D. Is it worth investing in mental health promotion and prevention of mental illness? A systematic review of the evidence from economic evaluations. BMC Public Health. (2008) 8:1–11. 10.1186/1471-2458-8-20 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Mrazek PJ, Haggerty RJ. Institute of Medicine (US) Committee on Prevention of Mental Disorders. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academies Press (US) (1994). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK236319/ (accessed March 2, 2022). [ PubMed ] [ Google Scholar ]
- 49. Meyer A. The mental hygiene movement. Can Med Assoc J. (1918) 8:632–4. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Cambridge . Prevention Meaning in the Cambridge English Dictionary. (2022). Available online at: https://dictionary.cambridge.org/dictionary/english/prevention (accessed March 2, 2022).
- 51. Baumann LC, Karel A. Prevention: primary, secondary, tertiary. In: Gellman MD, Turner JR, editors, Encyclopedia of Behavioral Medicine. New York, NY: Springer; (2013). p. 1532–4. Available online at: 10.1007/978-1-4419-1005-9_135 (accessed March 2, 2022). [ DOI ] [ Google Scholar ]
- 52. Commonwealth Department of Health and Aged Care . Introduction. In: Rickwood D. editor. Promotion, Prevention and Early Intervention for Mental Health – A Monograph. Canberra: Mental Health and Special Programs Branch, Commonwealth Department of Health and Aged Care; (2000). p. 1–8. [ Google Scholar ]
- 53. Hodgson R, Abbasi T, Clarkson J. Effective mental health promotion: a literature review. Health Educ J. (1996) 55:55–74. 10.1177/001789699605500106 [ DOI ] [ Google Scholar ]
- 54. Sartorius N. Health promotion strategies: keynote address. Can J Public Health Rev Can Santee Publique. (1988) 79:S3–5. [ PubMed ] [ Google Scholar ]
- 55. Jané-Llopis E, Hosman C, Jenkins R, Anderson P. Predictors of efficacy in depression prevention programmes. Meta-analysis. Br J Psychiatry J Ment Sci. (2003) 183:384–97. 10.1192/bjp.183.5.384 [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. World Health Organization . Prevention of Mental Disorders: Effective Interventions and Policy Options: Summary Report [cited 2022 Mar 5] (2004). [ Google Scholar ]
- 57. Min JA, Lee CU, Lee C. Mental health promotion and illness prevention: a challenge for psychiatrists. Psychiatry Investig. (2013) 10:307. 10.4306/pi.2013.10.4.307 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford University Press; (2005). Available online at: https://econpapers.repec.org/bookchap/oxpobooks/9780198529453.htm (accessed March 5, 2022). [ Google Scholar ]
- 59. Wanless D. Securing Good Health for the Whole Population: Population Health Trends. London: HM Treasury; (2003). p. 51. [ Google Scholar ]
- 60. Brady M, Assaad R, Ibrahim B, Salem A, Salem R, Zibani N. Providing New Opportunities to Adolescent Girls in Socially Conservative Settings: The Ishraq Program in Rural Upper Egypt—Full Report. Poverty Gend Youth. (2007) Available online at: https://knowledgecommons.popcouncil.org/departments_sbsr-pgy/226 (accessed March 15, 2022). [ Google Scholar ]
- 61. The Lancet Commission on Dementia Prevention Intervention Care: a call for action . Irish Journal of Psychological Medicine. Cambridge Core. (2021). Available online at: https://www.cambridge.org/core/journals/irish-journal-of-psychological-medicine/article/lancet-commission-on-dementia-prevention-intervention-and-care-a-call-for-action/3E7ED3B3B08161D9FC2B75FD8268703D (accessed May 21, 2022). [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. Balaji M, Andrews T, Andrew G, Patel V. The acceptability, feasibility, and effectiveness of a population-based intervention to promote youth health: an exploratory study in Goa, India. J Adolesc Health Off Publ Soc Adolesc Med. (2011) 48:453–60. 10.1016/j.jadohealth.2010.07.029 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 63. Rivet-Duval E, Heriot S, Hunt C. Preventing adolescent depression in mauritius: a universal school-based program. Child Adolesc Ment Health. (2011) 16:86–91. 10.1111/j.1475-3588.2010.00584.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Holen S, Waaktaar T, Lervåg A, Ystgaard M. The effectiveness of a universal school-based programme on coping and mental health: a randomised, controlled study of Zippy's Friends. Educ Psychol. (2012) 32:657–77. 10.1080/01443410.2012.686152 [ DOI ] [ Google Scholar ]
- 65. Loughry M, Ager A, Flouri E, Khamis V, Afana AH, Qouta S. The impact of structured activities among Palestinian children in a time of conflict. J Child Psychol Psychiatry. (2006) 47:1211–8. 10.1111/j.1469-7610.2006.01656.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Qouta SR, Palosaari E, Diab M, Punamäki RL. Intervention effectiveness among war-affected children: a cluster randomized controlled trial on improving mental health. J Trauma Stress. (2012) 25:288–98. 10.1002/jts.21707 [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Karam EG, Fayyad J, Nasser Karam A, Cordahi Tabet C, Melhem N, Mneimneh Z, et al. Effectiveness and specificity of a classroom-based group intervention in children and adolescents exposed to war in Lebanon. World Psychiatry Off J World Psychiatr Assoc WPA. (2008) 7:103–9. 10.1002/j.2051-5545.2008.tb00170.x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, et al. Impact of Stepping Stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. (2008) 337:a506. 10.1136/bmj.a506 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 69. Mishara BL, Ystgaard M. Effectiveness of a mental health promotion program to improve coping skills in young children: Zippy's Friends. Early Child Res Q. (2006) 21:110–23. 10.1016/j.ecresq.2006.01.002 [ DOI ] [ Google Scholar ]
- 70. Nielsen L, Meilstrup C, Nelausen MK, Koushede V, Holstein BE. Promotion of social and emotional competence: Experiences from a mental health intervention applying a whole school approach. Health Educ. (2015) 115:339–56. 10.1108/HE-03-2014-0039 [ DOI ] [ Google Scholar ]
- 71. Lange-Nielsen II, Kolltveit S, Thabet AAM, Dyregrov A, Pallesen S, Johnsen TB, et al. Short-term effects of a writing intervention among adolescents in Gaza. J Loss Trauma. (2012) 17:403–22. 10.1080/15325024.2011.650128 [ DOI ] [ Google Scholar ]
- 72. Mueller J, Alie C, Jonas B, Brown E, Sherr L. A quasi-experimental evaluation of a community-based art therapy intervention exploring the psychosocial health of children affected by HIV in South Africa. Trop Med Int Health TM IH. (2011) 16:57–66. 10.1111/j.1365-3156.2010.02682.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Bell CC, Bhana A, Petersen I, McKay MM, Gibbons R, Bannon W, et al. Building protective factors to offset sexually risky behaviors among black youths. J Natl Med Assoc. (2008) 100:936–44. 10.1016/S0027-9684(15)31408-5 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 74. Bonhauser M, Fernandez G, Püschel K, Yañez F, Montero J, Thompson B, et al. Improving physical fitness and emotional well-being in adolescents of low socioeconomic status in Chile: results of a school-based controlled trial. Health Promot Int. (2005) 20:113–22. 10.1093/heapro/dah603 [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Ager A, Akesson B, Stark L, Flouri E, Okot B, McCollister F, et al. The impact of the school-based Psychosocial Structured Activities (PSSA) program on conflict-affected children in northern Uganda. J Child Psychol Psychiatry. (2011) 52:1124–33. 10.1111/j.1469-7610.2011.02407.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Caldarella P, Christensen L, Kramer TJ, Kronmiller K. Promoting social and emotional learning in second grade students: a study of the strong start curriculum. Early Child Educ J. (2009) 37:51–6. 10.1007/s10643-009-0321-4 [ DOI ] [ Google Scholar ]
- 77. Yamamoto T, Matsumoto Y, Bernard ME. Effects of the cognitive-behavioral you can do it! Education program on the resilience of Japanese elementary school students: a preliminary investigation. Int J Educ Res. (2017) 86:50–8. 10.1016/j.ijer.2017.08.006 [ DOI ] [ Google Scholar ]
- 78. Neumann L, Dapp U, Jacobsen W, van Lenthe F, von Renteln-Kruse W. The MINDMAP project: mental well-being in urban environments. Z Gerontol Geriatr. (2017) 50:588–602. 10.1007/s00391-017-1290-7 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Ebert DD, Cuijpers P, Muñoz RF, Baumeister H. Prevention of mental health disorders using internet- and mobile-based interventions: a narrative review and recommendations for future research. Front Psychiatry. (2017) 8:116. 10.3389/fpsyt.2017.00116 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 80. Sharma A, Sharma SD, Sharma M. Mental health promotion: a narrative review of emerging trends. Curr Opin Psychiatry. (2017) 30:339–45. 10.1097/YCO.0000000000000347 [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Epstein I. Adventure therapy: a mental health promotion strategy in pediatric oncology. J Pediatr Oncol Nurs. (2004) 21:103–10. 10.1177/1043454203262684 [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. Natale P, Palmer SC, Ruospo M, Saglimbene VM, Rabindranath KS, Strippoli GF. Psychosocial interventions for preventing and treating depression in dialysis patients. Cochrane Database Syst Rev. (2019) 2019:CD004542. 10.1002/14651858.CD004542.pub3 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 83. Naslund JA, Aschbrenner KA. Digital technology for health promotion: opportunities to address excess mortality in persons living with severe mental disorders. Evid Based Ment Health. (2019) 22:17–22. 10.1136/ebmental-2018-300034 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 84. Ebert D, Erbe D. Internet-basierte psychologische interventionen. In: Berking M, Rief W. editors, Klinische Psychologie und Psychotherapie für Bachelor. Berlin; Heidelberg: Springer; (2012). p. 131–40. 10.1007/978-3-642-25523-6_12 [ DOI ] [ Google Scholar ]
- 85. Golkaramnay V, Bauer S, Haug S, Wolf M, Kordy H. The exploration of the effectiveness of group therapy through an Internet chat as aftercare: a controlled naturalistic study. Psychother Psychosom. (2007) 76:219–25. 10.1159/000101500 [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Kok G, Bockting C, Burger H, Smit F, Riper H. Mobile Cognitive Therapy: adherence and acceptability of an online intervention in remitted recurrently depressed patients. Internet Interv. (2014) 1:65–73. 10.1016/j.invent.2014.05.002 [ DOI ] [ Google Scholar ]
- 87. Olds DL, Hill PL, O'Brien R, Racine D, Moritz P. Taking preventive intervention to scale: the nurse-family partnership. Cogn Behav Pract. (2003) 10:278–90. 10.1016/S1077-7229(03)80046-9 [ DOI ] [ Google Scholar ]
- 88. Estrada S. Families healing together: exploring a family recovery online course. Qual Rep. (2016) 21:1216–1231. 10.46743/2160-3715/2016.2181 [ DOI ] [ Google Scholar ]
- 89. Forsman A, Nordmyr J, Park A, Matosevic T, McDaid D, Wahlbeck K. Technology-based interventions for mental health promotion in later life: an evidence review: Anna Forsman. Eur J Public Health. (2016) 26(Suppl.1):ckw172.044. 10.1093/eurpub/ckw172.044 [ DOI ] [ Google Scholar ]
- 90. Kutcher S, Bagnell A, Wei Y. Mental health literacy in secondary schools: a Canadian approach. Child Adolesc Psychiatr Clin N Am. (2015) 24:233–44. 10.1016/j.chc.2014.11.007 [ DOI ] [ PubMed ] [ Google Scholar ]
- 91. Mok K, Donovan R, Hocking B, Maher B, Lewis R, Pirkis J. Stimulating community action for suicide prevention: findings on the effectiveness of the Australian R U OK? Campaign Int J Ment Health Promot. (2016) 18:213–21. 10.1080/14623730.2016.1209423 [ DOI ] [ Google Scholar ]
- 92. Jorm AF, Christensen H, Griffiths KM. The impact of beyondblue: the national depression initiative on the Australian public's recognition of depression and beliefs about treatments. Aust N Z J Psychiatry. (2005) 39:248–54. 10.1080/j.1440-1614.2005.01561.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. Lindenberg K, Kordy H. Wirksamkeit eines gestuften, Internetvermittelten Ansatzes zur Prävention von Essstörungen bei Schülern der 7. bis 10. Klasse Kindh Entwickl. (2015) 24:55–63. 10.1026/0942-5403/a000152 [ DOI ] [ Google Scholar ]
- 94. Christensen H, Batterham PJ, Gosling JA, Ritterband LM, Griffiths KM, Thorndike FP, et al. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): a randomised controlled trial. Lancet Psychiatry. (2016) 3:333–41. 10.1016/S2215-0366(15)00536-2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 95. Bauer S, Wolf M, Haug S, Kordy H. The effectiveness of internet chat groups in relapse prevention after inpatient psychotherapy. Psychother Res J Soc Psychother Res. (2011) 21:219–26. 10.1080/10503307.2010.547530 [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. Buntrock C, Ebert DD, Lehr D, Cuijpers P, Riper H, Smit F, et al. Evaluating the efficacy and cost-effectiveness of web-based indicated prevention of major depression: design of a randomised controlled trial. BMC Psychiatry. (2014) 14:25. 10.1186/1471-244X-14-25 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 97. Imamura K, Kawakami N, Furukawa TA, Matsuyama Y, Shimazu A, Umanodan R, et al. Does Internet-based cognitive behavioral therapy (iCBT) prevent major depressive episode for workers? A 12-month follow-up of a randomized controlled trial. Psychol Med. (2015) 45:1907–17. 10.1017/S0033291714003006 [ DOI ] [ PubMed ] [ Google Scholar ]
- 98. Thompson NJ, Patel AH, Selwa LM, Stoll SC, Begley CE, Johnson EK, et al. Expanding the efficacy of project UPLIFT: distance delivery of mindfulness-based depression prevention to people with epilepsy. J Consult Clin Psychol. (2015) 83:304–13. 10.1037/a0038404 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 99. Naslund JA, Shidhaye R, Patel V. Digital technology for building capacity of nonspecialist health workers for task sharing and scaling up mental health care globally. Harv Rev Psychiatry. (2019) 27:181–92. 10.1097/HRP.0000000000000217 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 100. Maron E, Baldwin DS, Balõtšev R, Fabbri C, Gaur V, Hidalgo-Mazzei D, et al. Manifesto for an international digital mental health network. Digit Psychiatry. (2019) 2:14–24. 10.1080/2575517X.2019.1617575 [ DOI ] [ Google Scholar ]
- 101. Antonova E, Schlosser K, Pandey R, Kumari V. Coping with COVID-19: mindfulness-based approaches for mitigating mental health crisis. Front Psychiatry. (2021) 2021:563417. 10.3389/fpsyt.2021.563417 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 102. Stansfeld SA, Berney L, Bhui K, Chandola T, Costelloe C, Hounsome N. Pilot Study of a Randomised Trial of a Guided E-Learning Health Promotion Intervention for Managers Based on Management Standards for the Improvement of Employee Well-Being Reduction of Sickness Absence: The GEM (Guided E-learning for Managers) Study. Public Health Research. Southampton: NIHR Journals Library; (2015). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK310357/ (accessed February 22, 2022). [ PubMed ] [ Google Scholar ]
- 103. Carty S, Thompson L, Berger S, Jahnke K, Llewellyn R. Books on Prescription - community-based health initiative to increase access to mental health treatment: an evaluation. Aust N Z J Public Health. (2016) 40:276–8. 10.1111/1753-6405.12507 [ DOI ] [ PubMed ] [ Google Scholar ]
- 104. Nicholson J, Carpenter-Song EA, MacPherson LH, Tauscher JS, Burns TC, Lord SE. Developing the WorkingWell mobile app to promote job tenure for individuals with serious mental illnesses. Psychiatr Rehabil J. (2017) 40:276–82. 10.1037/prj0000201 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 105. Dawson SL, Dash SR, Jacka FN. The importance of diet and gut health to the treatment and prevention of mental disorders. Int Rev Neurobiol. (2016) 131:325–46. 10.1016/bs.irn.2016.08.009 [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry. (2015) 49:1087–206. 10.1177/0004867415617657 [ DOI ] [ PubMed ] [ Google Scholar ]
- 107. Michel T, Slovak P, Fitzpatrick G. An explorative review of youth mental health apps for prevention and promotion. In: Proceedings of the 13th EAI International Conference on Pervasive Computing Technologies for Healthcare - Demos and Posters. Trento: EAI; (2019). Available online at: http://eudl.eu/doi/10.4108/eai.20-5-2019.2283578 (accessed February 16, 2022). [ Google Scholar ]
- 108. King M, Bottomley C, Bellón-Saameño JA, Torres-Gonzalez F, Švab I, Rifel J, et al. An international risk prediction algorithm for the onset of generalized anxiety and panic syndromes in general practice attendees: predictA. Psychol Med. (2011) 41:1625–39. 10.1017/S0033291710002400 [ DOI ] [ PubMed ] [ Google Scholar ]
- 109. Wang J, Sareen J, Patten S, Bolton J, Schmitz N, Birney A, et al. prediction algorithm for first onset of major depression in the general population: development and validation. J Epidemiol Community Health. (2014) 68:418–24. 10.1136/jech-2013-202845 [ DOI ] [ PubMed ] [ Google Scholar ]
- 110. Insel TR, Scolnick EM. Cure therapeutics and strategic prevention: raising the bar for mental health research. Mol Psychiatry. (2006) 11:11–7. 10.1038/sj.mp.4001777 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 111. Segman RH, Shefi N, Goltser-Dubner T, Friedman N, Kaminski N, Shalev AY. Peripheral blood mononuclear cell gene expression profiles identify emergent post-traumatic stress disorder among trauma survivors. Mol Psychiatry. (2005) 10:500–13. 10.1038/sj.mp.4001636 [ DOI ] [ PubMed ] [ Google Scholar ]
- 112. Bockting CL, Kok GD, Kamp L, van der Smit F, van Valen E, Schoevers R, et al. Disrupting the rhythm of depression using Mobile Cognitive Therapy for recurrent depression: randomized controlled trial design and protocol. BMC Psychiatry. (2011) 11:12. 10.1186/1471-244X-11-12 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- View on publisher site
- PDF (574.5 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
- We're Hiring!
- Help Center
Mental Disorders
- Most Cited Papers
- Most Downloaded Papers
- Newest Papers
- Last »
- Psychiatry Follow Following
- Mental Disorder Follow Following
- Social Psychiatry Follow Following
- Sustainable forest management Follow Following
- Differential Diagnosis Follow Following
- Culture-Bound Syndromes Follow Following
- Stereotyping Follow Following
- Clinical Psychology Follow Following
- Mental Illness Follow Following
- Child Psychiatry Follow Following
Enter the email address you signed up with and we'll email you a reset link.
- Academia.edu Journals
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Psychiatric disorders articles from across Nature Portfolio
Psychiatric disorders are a heterogeneous group of mental disorders, manifesting as unusual mental or behavioural patterns that cause distress or disability to the individual.
Related Subjects
- Autism spectrum disorders
- Bipolar disorder
- Obsessive compulsive disorder
- Post-traumatic stress disorder
- Schizophrenia
Latest Research and Reviews

Amygdala intercalated cells form an evolutionarily conserved system orchestrating brain networks
This comprehensive review of amygdala intercalated cells (ITCs) proposes a revised model of ITCs as a highly coordinated system that integrates diverse inputs to orchestrate brain-wide networks and shape behavioral states.
- Ayla Aksoy-Aksel
- Francesco Ferraguti
- Ingrid Ehrlich
Heterogeneous patterns of brain atrophy in schizophrenia localize to a common brain network
Utilizing heterogeneous results from the published studies on brain atrophy in schizophrenia, the authors identify a common brain network for schizophrenia that is stable with disease progression and across different clusters of schizophrenia symptoms.
- Ahmed T. Makhlouf
- William Drew
- Shan H. Siddiqi
Acute cannabidiol administration reduces alcohol craving and cue-induced nucleus accumbens activation in individuals with alcohol use disorder: the double-blind randomized controlled ICONIC trial
- Sina Zimmermann
- Anton Teetzmann
- Patrick Bach
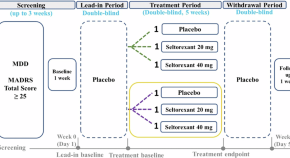
Treatment effect and safety of seltorexant as monotherapy for patients with major depressive disorder: a randomized, placebo-controlled clinical trial
- Sofie Mesens
- Wayne C. Drevets
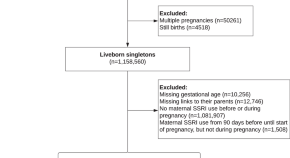
Prenatal exposure to selective serotonin reuptake inhibitors and risk of disorders of gut-brain interaction in children
- Helene Kildegaard
- Mette Bliddal
- Ardesheer Talati

Gut microbiota regulate insomnia-like behaviors via gut-brain metabolic axis
News and Comment
Supporting the sexual healthcare needs of aging women.
A satisfying sex life is a key component of health and well-being for many older women. However, there is insufficient awareness of and care for women’s sexual health. This Comment discusses steps healthcare providers can take to support women’s sexual health across the lifespan, which should be a top priority.
- Holly N. Thomas
Reply to “Letter to the Editor regarding ‘Unique pharmacodynamic properties and low abuse liability of the μ-opioid receptor ligand (S)-methadone’”
- Marjorie R. Levinstein
- Paulo A. De Oliveira
- Michael Michaelides

Stress can dull our capacity for joy: mouse brain patterns hint at why
Scientists pinpoint brain circuits linked to either resilience or vulnerability to adversity, which affect a stressed animal’s pursuit of pleasure.

Evaluating the safety of orexin receptor antagonists on reproductive health and sexual function
- Kenji Hashimoto

Internet use linked to better mental health in older adults
According to a large international study, Internet use among adults 50 or more years of age correlates with reduced depressive symptoms, increased life satisfaction and improved self-reported health.
- Karen O’Leary

New schizophrenia drug could treat Alzheimer’s disease
Half a dozen drugs are in trials for conditions of the brain, but success is not guaranteed.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
The social determinants of mental health and disorder: evidence, prevention and recommendations
Affiliations.
- 1 Division of Psychiatry, University College London, London, UK.
- 2 City College, City University of New York, New York, NY, USA.
- 3 Graduate Center, City University of New York, New York, NY, USA.
- 4 School of Epidemiology and Public Health, University of Ottawa, Ottawa, ON, Canada.
- 5 Department of Psychiatry, University of Cambridge, Cambridge, UK.
- 6 Cambridgeshire & Peterborough NHS Foundation Trust, Cambridge, UK.
- 7 Medical Research Council Unit for Lifelong Health and Ageing, University College London, London, UK.
- 8 Centre for Longitudinal Studies, Social Research Institute, University College London, London, UK.
- 9 Camden and Islington NHS Foundation Trust, London, UK.
- 10 Department of Psychiatry, University of Oxford, Oxford, UK.
- 11 Institute for Mental Health, University of Birmingham, Birmingham, UK.
- PMID: 38214615
- PMCID: PMC10786006
- DOI: 10.1002/wps.21160
People exposed to more unfavourable social circumstances are more vulnerable to poor mental health over their life course, in ways that are often determined by structural factors which generate and perpetuate intergenerational cycles of disadvantage and poor health. Addressing these challenges is an imperative matter of social justice. In this paper we provide a roadmap to address the social determinants that cause mental ill health. Relying as far as possible on high-quality evidence, we first map out the literature that supports a causal link between social determinants and later mental health outcomes. Given the breadth of this topic, we focus on the most pervasive social determinants across the life course, and those that are common across major mental disorders. We draw primarily on the available evidence from the Global North, acknowledging that other global contexts will face both similar and unique sets of social determinants that will require equitable attention. Much of our evidence focuses on mental health in groups who are marginalized, and thus often exposed to a multitude of intersecting social risk factors. These groups include refugees, asylum seekers and displaced persons, as well as ethnoracial minoritized groups; lesbian, gay, bisexual, transgender and queer (LGBTQ+) groups; and those living in poverty. We then introduce a preventive framework for conceptualizing the link between social determinants and mental health and disorder, which can guide much needed primary prevention strategies capable of reducing inequalities and improving population mental health. Following this, we provide a review of the evidence concerning candidate preventive strategies to intervene on social determinants of mental health. These interventions fall broadly within the scope of universal, selected and indicated primary prevention strategies, but we also briefly review important secondary and tertiary strategies to promote recovery in those with existing mental disorders. Finally, we provide seven key recommendations, framed around social justice, which constitute a roadmap for action in research, policy and public health. Adoption of these recommendations would provide an opportunity to advance efforts to intervene on modifiable social determinants that affect population mental health.
Keywords: Mental health; marginalized groups; mental disorder; population mental health; prevention; social determinants; social justice; social risk factors.
© 2024 World Psychiatric Association.
Grants and funding
- WT_/Wellcome Trust/United Kingdom
- MC_UU_00019/3/MRC_/Medical Research Council/United Kingdom

IMAGES
VIDEO
COMMENTS
References. Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance. 1. Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010.
The National Institute of Mental Health (NIMH) is the Nation's leader in research on mental disorders, supporting research to transform the understanding and treatment of mental illnesses. Below you can learn more about NIMH funded research areas, policies, resources, initiatives, and research conducted by NIMH on the NIH campus.
The Mental Health Journal is a rigorously peer-reviewed scholarly publication dedicated to advancing the field of mental health research. Toggle navigation ... low compared to the potential cost savings associated with reduced hospitalizations for people with severe persistent mental illness. ... This paper reviews the existing literature and ...
In this paper, we describe and present the vast, fragmented, and complex literature related to this topic. This review may be used to guide practice, public health efforts, policy, and research related to mental health and, specifically, depression. Keywords: depression, major depressive disorder, risk factor, protective factor, determinant ...
Diagnostic and Statist ical Manual of Mental Disorders (DSM-5) and the International Classification of Diseases (ICD-11 ), provide standardized criteria for diagnosing psychiatric diso rders [21,22].
Instead, greater emphasis has been given to the illness aspect, such as research on psychopathology, mental disorders, and treatment (19, 20). Often, physicians and psychiatrists are unfamiliar with various concepts, approaches, ... Additionally, we included original papers from the last 5 years (2016-2021) so that they do not get missed out ...
Public stigma against people with mental health problems is damaging to individuals with mental illness and is associated with substantial societal burden. 1,2 It is a global phenomenon, 3 which is prevalent and persists over time. 4,5 A recent systematic review and meta-analysis of public attitudes showed that despite improvements in mental ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on PSYCHOLOGICAL DISORDERS. ... There is a growing tendency for mental health disorders to emerge during ...
Psychiatric disorders are a heterogeneous group of mental disorders, manifesting as unusual mental or behavioural patterns that cause distress or disability to the individual. Related Subjects ...
Addressing these challenges is an imperative matter of social justice. In this paper we provide a roadmap to address the social determinants that cause mental ill health. Relying as far as possible on high-quality evidence, we first map out the literature that supports a causal link between social determinants and later mental health outcomes.