
Transforming the understanding and treatment of mental illnesses.
Información en español
- About the Acting NIMH Director
- Advisory Boards and Groups
- Strategic Plan
- Offices and Divisions
- Careers at NIMH
- Staff Directories
- Getting to NIMH

Stigma and Discrimination Research Toolkit

The Stigma and Discrimination Research toolkit is a collection of evidence and resources related to stigma and discrimination research. Health-related stigma and discrimination research has produced theories, models, frameworks, measures, methods, and interventions that can be applied across conditions and populations to help reduce the impact of stigma and discrimination.
This toolkit may be helpful for researchers, government officials looking to incorporate research into policy, community agencies, and various other stakeholders across disciplines and sectors. This toolkit includes a special emphasis for those looking to address stigma and discrimination issues related to the coronavirus (COVID-19) pandemic.
This toolkit was developed by NIMH, in partnership with the Fogarty International Center (FIC), the National Institute on Drug Abuse (NIDA), and the NIH Stigma Scientific Interest Group.
Note: These resources are provided for informational purposes only. These are not comprehensive lists and do not constitute an endorsement by NIMH, FIC, NIDA, the National Institutes of Health, the U.S. Department of Health and Human Services, or the U.S. government.
About Stigma
Stigma is a social phenomenon that involves negative attitudes (prejudices) or beliefs (stereotypes) about others typically (but not always) based on defining characteristics such as sexuality or health conditions (e.g., HIV, mental illness, or substance use) that are perceived to be contagious, dangerous, or incurable. It is relational in nature as occurring in the context of power. Goffman defined stigma as “an attribute that is deeply discrediting” that reduces the individual “from a whole and usual person to a tainted, discounted one.” [1] Stigma and the process of stigmatization consists of identifying and labeling a “difference,” linking a labeled person to undesirable characteristics, and separating “them” from “us”; thus, the stigmatized group (“them”) subsequently experiences discrimination and loss of status in the context of social, economic and political power. For example:
- Health-related stigma happens when people have or are associated with a specific health condition perceived as undesirable. As a result of this stigma, they may avoid seeking screening or treatment or are treated differently or poorly by others because of it.
- Health-related discrimination is discrimination based on a health condition, disease, or another health-related issue. It may occur in the workplace, health care, education, housing, and other settings.
There are multiple types of health-related stigma, including:
- Internalized stigma: The individual believes they are bad or at fault for having a health condition
- Enacted stigma: The individual experiences discrimination from others because they are known or believed to have a health condition
- Anticipated stigma: The individual expects or fears future discrimination due to the health condition
- Associated stigma: Others, such as family members or healthcare workers, experience discrimination because of their proximity to those with a health condition.
- Perceived stigma: An individual’s perceptions about how stigmatized groups are treated due to a health condition.
Stigma exists at multiple levels:
- Individual level: A person’s cognitive, affective, and behavioral responses to facing or experiencing stigma, including concealment and disclosure, internalization, and stigma consciousness
- Interpersonal level: Discrimination as expressed by one person toward another, manifesting in ways such as lack of respect, devaluation, and dehumanization
- Structural level: Societal-level conditions, cultural norms, and institutional policies that constrain the opportunities, resources, and well-being of the stigmatized [ 2 ]
Stigma’s Impact on Health
Research shows that health-related stigma for any condition is not just a social problem. It can have detrimental impacts on how health care is sought, accessed, and delivered, and slow scientific progress. Stigma is also associated with poor health outcomes and reduced service utilization. For example, stigma related to conditions like HIV, tuberculosis, epilepsy, and substance use, increases the likelihood that the individual will develop a related mental disorder like depression or anxiety. In addition, research shows that stigma reduces quality of life and makes individuals less likely to seek out needed care.
Language and Stigma
The language we use to talk about health plays a crucial role in shaping opinions and beliefs about a disease or condition, and the people affected. Scientific and medical terminology typically used by the research community may inadvertently create or perpetuate stereotypes about diseases or drive fear and “othering.”
Proactively using language that empowers individuals and communities, and takes patient experience into account, can help individuals communicate about health in a non-stigmatizing way. The below language guides offer examples.
- National Institute of Allergy and Infectious Diseases (NIAID) HIV Language Guide : This guide includes language suggestions for communicating about HIV and related topics. The Language Guide describes current thinking and best practices and procedures. It aims to help scientists, administrators, and researchers use fair, accurate, and respectful language and aid funded research networks, sites, centers, investigators, and stakeholders as they draft protocols and develop communications and outreach materials.
- National Institute on Drug Abuse (NIDA) Preferred Language for Talking About Addiction : Addiction is a chronic but treatable health condition. Often unintentionally, many people still talk about addiction in ways that are stigmatizing—meaning they use words that can portray someone with a substance use disorder (SUD) in a shameful or negative way that may prevent individuals from seeking treatment for SUDs. With simple changes in language, stigma and negativity around SUDs can be reduced or avoided. This resource discusses what stigma is, how it affects people with SUD, and how to change language usage.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Effects of mental health stigma on loneliness, social isolation, and relationships in young people with depression symptoms
Katie prizeman, netta weinstein, ciara mccabe.
- Author information
- Article notes
- Copyright and License information
Corresponding author.
Received 2023 Mar 28; Accepted 2023 Jun 30; Collection date 2023.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Major depressive disorder (MDD) is the most prevalent affective disorder and the leading cause of illness and disability among young people worldwide. Besides being more susceptible to the onset of depression, young people have a higher risk of loneliness, and their personal and social development is impacted by social relationships during this time. It is thought that mental health stigma can undermine both help-seeking and longer-term outcomes for disorders like depression in young people. However, how stigma (i.e., related to depression) might affect young people’s feelings of loneliness, social isolation, and relationships is unclear. Using qualitative research methods, this study aimed to explore the subjective experiences of public and internalized stigma and its effects on loneliness, social isolation, and relationship quality in young people with depression symptoms.
We carried out in-depth, semi-structured interviews with N = 22 young people aged 17–25 (M age = 22 years) who reported high symptoms of depression (Mood and Feelings Questionnaire (MFQ) score > 27) (i.e., community sample, N = 9) or had been previously diagnosed with depression by a medical professional (i.e., clinical sample, N = 13). Data were analysed using thematic analysis. We explored the subjective effects of depression stigma on loneliness, social isolation, and relationships.
Participants described both public stigma (i.e., initiated by others) and internalized stigma (i.e., self-imposed) as disrupting social relationships and eliciting loneliness, isolation, and depressive symptomology. Four main themes about young people's subjective experiences of stigma were identified: 1) Others’ Misunderstanding of Mental Health Disorders and the Impact Misunderstanding has on Relationships ; 2) Effects of Stigma on the Self and Wellbeing ; 3) Stigma Fosters Secrecy Versus Disclosure ; and 4) Stigma Increases Loneliness Driven by Avoidance of Social Contexts .
Conclusions
Young people's accounts revealed a wide range of consequences beyond their depression diagnosis. Participants often felt discriminated against, misunderstood, and judged by others as a result of public stigma; they discussed internalizing these attitudes. They suggested that a lack of understanding from others, for example from their partners, family, and peers, and unreliable and/or absent support systems resulted in increased feelings of loneliness and social isolation and reduced the quality and quantity of relationship formation, social bonds, and interactions. Stigma also reduced their self-esteem and confidence, which in turn fostered secrecy and a reluctance to disclose their depression. Despite depression's stigma, most participants reported having long-term goals and aspirations to reconnect with others. These goals stood in contrast to feeling hopeless and unmotivated during periods of depression. Overall, we reveal how stigma can impact feelings of loneliness, social isolation, and relationships among young people with depression, which could lead to targeted interventions to lessen the impact of stigma in this population.
Keywords: Depression, Mental health stigma, Loneliness, Social isolation, Subjective experiences, Young people, Qualitative research
Major depressive disorder (MDD) is the most prevalent affective disorder and the leading cause of illness and disability among young people worldwide [ 18 , 81 , 71 , 92 , 95 ]. Young people aged 17 to 18 had a lifetime prevalence of 15.4% [ 71 ], comparable to that of young adults and older people, who showed a median 12-month prevalence estimate of approximately between 4 and 7.5% [ 4 ]. Besides being considered a major disease burden [ 100 ], MDD is also linked to long-term vulnerability, which may negatively affect young people's development [ 36 , 101 ]. Young people who have experienced at least one depressive episode are more likely to experience long-term adverse health, economic, and social impacts [ 17 ], increased hospitalizations, suicide rates [ 48 ], and high rates of recurrence during adulthood [ 33 , 35 , 39 ]. There are direct links between youth depression and subsequent mental health difficulties [ 68 ], but it is also clear that the social context matters: the extent to which young people with MDD are supported by others influences the impact of the diagnosis on their mental health and wellbeing over time [ 56 , 65 ]. It is imperative to understand why this might be and how we can encourage young people to seek help and find support.
Stigma may undermine mental health and wellbeing over time through its detrimental effects on social relationships; we posit that this is a key concern for understanding stigma in depressed youths. In addition to being more susceptible to depression, young people also have a higher risk of loneliness [ 1 ]. Loneliness develops when there is a perceived imbalance between desired and actual social connections [ 66 ], which impacts young people’s quality of life, illness prognosis, and willingness to seek care [ 86 ]. Whereas solitude suggests a desire to be alone and is fundamentally neutral, both loneliness and social isolation for extended periods of time are distinctly negative experiences [ 30 ]. Notably, individuals in solitude do not inevitably experience loneliness [ 70 ], and lonely young people do not always spend less time with other people compared to less lonely people [ 14 ].
Previous quantitative work suggests links between loneliness, social isolation, and depression in the younger population [ 41 , 70 ]. However, there is a little qualitative knowledge of how these influence one another [ 1 ] and whether or not stigma experiences play a role in various aspects of relationships, including loneliness, social isolation, and withdrawal [ 37 , 59 , 96 ].
Stigma about mental illness is a broad concept comprised of negative stereotypes, prejudices (endorsement of stereotypes and emotional reactions), and discriminatory behaviours against people with mental health problems [ 22 , 85 ]. It can be understood when a person has lost status in society because of their mental health [ 26 , 42 , 51 ]. Stigma involves feelings of humiliation—that one is at fault, degraded, or the object of displeasure [ 3 , 54 , 106 ]—and leads to feeling devalued, rejected, and stressed [ 31 , 77 ].
When discussing stigma associated with mental health disorders, it is important to distinguish between two major forms of stigma: 1) public stigma and 2) internalized stigma [ 8 ]. Public stigma is when large groups of people in Western societies agree with negative stereotypes and act against or devalue people from certain social groups or classes, like those with mental health disorders [ 20 ]. Internalized stigma is when people have negative thoughts, beliefs, and stereotypes about their own conditions [ 21 , 24 ]. It is by becoming preoccupied with society’s prejudices and/or hostility that mentally ill individuals internalize these objectionable stereotypes [ 11 ].
Youth is a time for exploring oneself in relation to society and social contexts, as well as a key period for individuals to form strong relationships [ 27 , 49 ]. In the case of mental health stigma, young people with mental health difficulties may struggle to incorporate these experiences into their identity or to share these aspects of their identity with others for fear of rejection or hostility [ 12 , 72 ]. Previous research has shown that young people are subject to stigmatizing contexts and experiences that may be unique to their particular developmental challenges [ 74 ]. For example, the transitional period from childhood to adulthood is commonly known to be a sensitive period in which lived experiences can have profound long-term effects on future health and development [ 52 , 91 ].
Young people with depression must deal with those symptoms, but they are also challenged by associated stigma and possibly linked feelings of loneliness and isolation [ 23 , 88 ]. Stigma has been identified as a factor in the negative outcomes and wellbeing of young people with MDD [ 24 , 74 ]. It is possible that the reduced quality and quantity of relationships and social interactions, or lack thereof (i.e., social withdrawal), that are apparent in depression [ 65 ] could in part be due to stigma rather than the depression itself [ 12 , 72 ]. In particular, studies find that public and internalized stigma can negatively impact young people's development of a sense of self (i.e., self-identity, self-esteem, and self-worth), social relationships, and withdrawal [ 53 , 93 ]. Research into mental health stigma has largely focused on investigating this concept in adults [ 74 ], much less is known about young people with depressive symptoms and the stigma they experience [ 50 , 67 , 94 ]. More research is needed to better understand public and internalized stigma in these populations [ 32 , 38 ]. In particular, how stigma influences the loneliness and social relationships of youth depression is important to understand, as young people are at a developmental stage where social connections are key [ 81 , 84 ].
Research on how mental health stigma is experienced by young people with depression is limited [ 74 ], as is research on its impact on loneliness, social isolation, and relationships [ 69 ]. Taken together, conceptual frameworks are needed that describe how young people experience depression stigma and its impact on loneliness, social isolation, and relationships, given that these social experiences and emotions are key factors that influence young people's development into adulthood and that could worsen mental health outcomes [ 19 , 81 ].
In this study, we explore the subjective experiences of mental health stigma and its influence on feelings of loneliness, social isolation, and relationship experiences. To address research gaps, this study focused on two main research questions: 1) What are young people's subjective experiences of mental health stigma? and 2) How does stigma influence feelings of loneliness, social isolation, and relationship experiences in young people with depression symptoms? The age range of 17–25 years was selected to better understand this key early age in adult development that reflects the transition from adolescence to adulthood [ 61 , 87 ]. This age range focuses entirely on the younger population, also referred to as "young people".
This study's major aims are to establish the existing literature among young people in order to better understand their subjective stigma experiences as well as explore any effects stigma may have on experiences of loneliness, social isolation, and relationship experiences. To provide for flexibility and give young people a voice, semi-structured interviews with a number of open-ended questions were used. These questions allowed participants to direct a discussion based on personal experiences of stigma. Due to its more open-ended character, this interview technique adds more detail and richness, enabling us as researchers to identify patterns while still allowing comparisons between participants [ 58 ]. The primary objective of our approach is to provide young people's subjective experiences to inform the development of stigma research and awareness in order to prevent or minimize adverse stigmatizing experiences in young people with depression. Understanding young people's experiences with stigma and how it affects feelings of loneliness, social isolation, and relationships may help develop more effective targeted interventions that reduce stigmatizing attitudes and beliefs about depression.
Participants and recruitment
Participants' demographics and clinical characteristics are presented in Table 1 .
Participant demographics and clinical characteristics
MFQ Mood and Feelings Questionnaire (higher scores indicate more depression). All participants completed the long version of the MFQ
a Age at interview
b MFQ score at screening or diagnosis
Participant recruitment from the community involved emails to listservs, and the study strictly followed the standards of voluntary and informed consent and data protection for each participant who voluntarily fulfilled the inclusion criteria. Participants included 22 young people between the ages of 17 and 25 ( M = 22 years) who had high symptoms of depression or had been currently diagnosed by a medical professional. Fifteen of the 22 participants took part in the interview. There were no other inclusion or exclusion criteria. Depression symptoms were assessed through a pre-screen using the Mood and Feelings Questionnaire (MFQ) [ 25 ] with a benchmark score of > 27, administered by the primary researcher (KP) via an online survey prior to individuals taking part in the study. Of the sample, N = 13 had a current diagnosis of depression by a medical professional (Table 1 ).
Data collection
Mood and feelings questionnaire (mfq).
The MFQ is a 33-item scale that measures depressive symptoms in children and young adults. It has good psychometric properties [ 29 , 83 ]. Participants' responses indicate how they have been feeling or acting in the past two weeks [ 25 ]. A cut-off score of 27 and above has been identified as the difference between clinical and non-clinical levels of depressive symptoms [ 105 ]. Each item is rated on a three-point Likert scale from 0 ( not true ) to 2 ( true ). This questionnaire is widely used to score depression in young people, with higher scores suggesting more depression symptomatology [ 105 ].
Semi-structured interviews
Using their clinical and research expertise in the fields of mental health stigma, MDD, loneliness, social isolation, and relationship experiences, the authors created a semi-structured interview schedule to guide discussions (Table 2 ). Participants completed demographic questions regarding age, gender, education, geographical location, and ethnicity prior to semi-structured interviews. Semi-structured interviews ( N = 22) were scheduled and conducted online (using the Microsoft Teams platform) with participants by KP between June 2022 and August 2022 (post-COVID-19 lockdown). Interviews were conducted until data saturation was reached, meaning that no new information was observed and collected [ 46 ]. Interviews were audio-recorded, transcribed verbatim, checked for accuracy, and subjected to thematic coding by KP. Each interview lasted between approximately 25 and 60 min and was conducted in English.
Qualitative interview guide
While some of the semi-structured interview questions mentioned direct concepts such as stigma, loneliness, and social isolation, other questions were more open-ended, allowing participants to describe these organically. Interview questions were piloted with young people aged 17–25 and revised as necessary. The topic guide explored the following: 1) broad/general mental health stigma experiences; 2) specific events recalled; and 3) recovery questions. Recovery questions were used to give participants an opportunity to talk about any other opinions or experiences they would like to share. See Table 2 for a summary of the qualitative interview guide.
The topic guide was used flexibly through a semi-structured interview and comprised interview questions relating to subjective experiences of mental health stigma, followed by prompts to gather richer data about each individual’s particular experience. The first author (KP) conducted all the interviews online. They took place online using the Microsoft Teams platform, in a quiet room with only the researcher and participant present. Interviews were audio recorded and lasted an average of 30 min (range 20–50 min). Participants were placed into a draw to receive a £40 gift voucher for their participation. Interviews were conducted until saturation was reached, such that the data collection process no longer offered any new or relevant insights [ 46 ]. Interviews were transcribed verbatim by KP. Field notes were made after the interview and used to aid analysis.
Data analysis
Thematic analysis (TA) was employed to identify and analyse patterns of meaning in the dataset. This technique is ideal for investigating how a group conceptualizes a particular phenomenon [ 47 ]. TA is not tied to a particular ontological or epistemological position,therefore, in this study, the researchers adopted a post-positivist critical realist stance [ 44 ]. This position assumes that reality is observable and quantifiable while recognizing that participants are unaware of all the factors that influence their experience [ 47 ]. Furthermore, to align this work with emerging literature on stigma experienced by people with mental health problems, we chose a pragmatist approach to materials and an abductive process of data analysis (i.e., inference to the best explanation allows inferring, such as "a" as an explanation of "b") [ 57 ]. Primarily, we used an inductive, “bottom-up” approach [ 78 ]. Without first attempting to fit the data into pre-existing coding schemes, the data were examined. That being said, we did not dismiss possible themes that did not fit current literature, nor did we identify themes unless they were evident in the data.
The researchers considered their own sources of bias and prior assumptions, including knowledge of depression and mental health stigma (KP), when conducting research into young people’s mental health (KP, CM, NW). The data were analysed using constant comparative techniques based on Braun and Clarke's six-stage TA method [ 10 ]. In stage 1), the first author (KP) familiarized themselves with the data by conducting and transcribing interviews and then rereading the transcripts. In stage 2), KP conducted line-by-line coding. The process of coding was inductive and iterative, with constant comparisons between and within transcripts. Initially, all data were coded for both explicit and implicit meanings. The labelling of codes focused on capturing the subjective experiences of mental health stigma as well as its implications for feelings of loneliness, social isolation, and further wellbeing concerns [ 55 , 97 ]. In stage 3), codes were combined into potential themes that reflected the data's major characteristics and patterns. In stages 4) and 5), themes were evaluated by examining all codes and themes in aggregate [ 10 , 45 ]. Tentative themes were reviewed by the research team (KP, CM, NW) [ 79 , 102 ]. During these coding meetings, alternative interpretations of patterns in the data were considered and discussed until a consensus was reached. In the final stage 6), themes were finalized, and quotations exemplifying each theme were identified.
See Table 3 for a summary of the themes discussed below. Similar viewpoints were shared by those with and without a formal depression diagnosis.
Table of themes and sub-themes
Overview of themes
Young people’s subjective experiences were captured in four main themes: 1) Others’ Misunderstanding of Mental Health Disorders and the Impact Misunderstanding has on Relationships ; 2) Effects of Stigma on the Self and Wellbeing ; 3) Stigma Fosters Secrecy Versus Disclosure ; and 4) Stigma Increases Loneliness Driven by Avoidance of Social Contexts (Table 3 ). Each theme highlighted a unique aspect of stigmatizing experiences; however, there were areas of conceptual overlap between themes. All major themes and sub-themes were expressed by both those with and without a depression diagnosis. Participants also expressed that internalized stigma was an antecedent to bigger problems, such as a lack of honesty and disclosure in relationships, poorly formed relationships, difficulties trusting and communicating, a negative self-identity, and low self-esteem. We explore these below: All themes were further defined by sub-themes that depicted the nature of conversations (Table 3 ).
Theme one: Others’ misunderstanding of mental health disorders and the impact misunderstanding has on relationships
During interviews, participants talked about how most of the people they had a relationship with did not understand their mental health conditions or what it meant to have a mental disorder. They said this affected their relationships and social interactions.
Sub-theme: Hallmark/typical symptoms associated with depression
“...when people experience depression, they kind of have very hallmark typical symptoms that people associated with it.” (P11, 25, Female)
Participants said that most people have a set idea of what depression is and what the common symptoms and stereotypes are. One of these ideas is that others think that depressed people are sad and suicidal. Participants also talked about how others see, talk about, and try to discredit MDD (for example, by claiming that MDD is not a real medical condition or is "nonsense"). Participants expressed that these stereotypes made them feel judged, undervalued, and misunderstood by others.
Participants felt that others did not understand what it meant to be diagnosed with depression or the signs of MDD. Participants expressed negative emotions such as shame and guilt as a result of others’ lack of understanding, and they reported that such misunderstanding negatively impacted the way they saw themselves (i.e., they experienced lowered self-confidence, self-esteem, and self-worth, as well as insecurities such as feelings of abnormality and weirdness). Participants knew that others cared for them but lacked education about, e.g., depression. Still, the majority of participants would choose not to invest in relationships with those who misunderstood them, as they felt that it would do more harm than good.
“So, like, I have this one friend. He doesn't have any mental health issues, but like when I talk to him, he, like, just doesn't quite say the right thing. But it's like, I know that that's just because he doesn't understand. Not because he doesn´t care.” (P02, 21, Female)
“...I've made that conscious choice to spend time with people who do care and at least try to understand.” (P02, 21, Female)
Participants reported that they were sometimes unable or found it difficult to make friends or communicate with others due to thinking or feeling that they were being judged by those around them. This made participants feel that others viewed them as crazy and abnormal, views they also came to believe (i.e., internalized). Once alone with their thoughts, some recognized that these thoughts and feelings may be a protection mechanism as a way to guard oneself from judgment, stigmatizing experiences, and stereotypical attitudes and beliefs. By avoiding getting close to others or forming relationships, participants were unable to experience victimization and also avoided the topic of mental health coming up in discussion. Some participants chose to continue isolating because it felt less painful than worrying about what others thought.
“And then, as you get to know each other more, you realize that it’s more and more important to talk about the way you feel. When that happens, your relationship inevitably changes. That’s quite hard…” (P21, 21, Male)
Sub-theme: Understanding acts as a support system
Some chose to talk about their mental health diagnosis with others with whom they felt comfortable and who had had similar experiences with depression. They did this to fight the silencing effects of stigma and to paint a more accurate picture of what it means to be diagnosed with depression. However, some felt that their self-disclosure furthered their own guilt and others’ blame for their mental illness, which in turn led to increased internalized stigma, secrecy, and self-identity problems, including low self-esteem. Such conversations created a further feeling of being stigmatized.
“...it is definitely still challenging talking to people about things like self-harm and what that means to people, I think is quite misunderstood. And with stigma, you just sort of... There’s a lot of stigmas there, really. And yeah, I think that’s definitely affected me as well.” (P06, 22, Female)
Participants also described having a positive social experience when they shared aspects of MDD. For instance, participants describe the positive influence sharing their experiences has if it is with others with similar experiences of MDD. They describe the positive effects of people who show care and support for individuals with mental illnesses and who have a better understanding of mental disorders. Participants expressed the positive influence that understanding, support, and care had on relationship bonds and their associated social interactions, as well as how they positively impacted their self-worth and wellbeing.
“Yeah, kind of because I feel like most of my friends have similar issues. So, I feel generally more understood. When I’m at home, I kind of just want to go be alone because I feel like people just don´t understand as much.” (P02, 21, Female)
“So, my mother, she takes it very personally because her mother was also diagnosed with depression and she committed suicide [sic]. So, my mother, it like scared her the first time I told her that I was diagnosed, but she was still very supporting… And my sister, she struggles with generalized anxiety disorder, so I think, she and I, we um, we support each other with medications. Um, like she is starting with new antidepressants now. So, we just we support each other. We like talk to each other, like, kind of experiencing kind of experiencing kind of the same thing in a way.” (P03, 24, Female)
Theme two: Effects of stigma on the self and wellbeing
Participants expressed that having a formal diagnosis made it harder for them to shake the feeling that they were not good enough or useful. Participants felt this unintentionally changed how they saw the “self” (i.e., lowered self-confidence, self-esteem, and self-worth), as well as the way they responded to being in social contexts. The majority of those interviewed stated that their own stigmatizing experiences started out in public and gradually became internalized over time.
“I tend to actually believe it when it’s stuff like that. It's more when they say things like, ´That's stupid for thinking that sort of thing.´ I think it´s supposed to be reassuring, like ´Oh, you don´t need to worry,´ but it´s kind of the way they say it, ´Ah, why you´re being so stupid for thinking that sort of thing?´ So yeah… stuff like that.” (P02, 21, Female)
Sub-theme: Diagnosis and self-identity
Participants expressed experiencing a decrease in self-esteem and self-worth after being diagnosed with a mental illness. Many participants said that their first diagnosis was a turning point in how their identity changed. Participants' self-destructive views and thoughts of the "self" began with feelings of weakness and insignificance, increased guilt, and a lack of empathy and kindness.
“I think the fact that before I was diagnosed, I also thought it was just a bunch of nonsense. I think in the beginning I was quite mad, um, I was dealing with it for such a long time, and I was also just thinking that this is nonsense. You know, when I was diagnosed, I was like, ´Okay, I’m one of those people now.´” (P03, 24, Female)
“It made me feel like I am the problem. I’ve always thought like I´m a problem and having someone else confirm it just made me feel worse because I try so hard, but at other times really, I struggle.” (P17, 22, Male)
A person's motivation, mental health, and overall quality of life can all be hurt by low self-esteem [ 5 , 34 ]. These key elements were expressed as negatively influencing one’s self-worth, self-esteem, and wellbeing and were recurring themes in participant interviews. Participants experienced decreased self-confidence, feelings of insecurity, a lack of identity, and feelings of not belonging.
“It certainly affects your self-esteem… there’s definitely something like that constant, almost like rumination of like, ´Are they judging me? Am I behaving normally? Like, are they gonna judge me if I cancel this because I am not feeling up to it?´...that kind of stuff.” (P11, 25, Female)
Only a small number of individuals took something positive out of receiving a diagnosis, such as unexpected insights and an appreciation of how essential one's mental health is to one's identity. Feelings of relief and recognition were also mentioned after receiving a diagnosis.
“Yeah, I think for myself, I felt that I wasn't as strong as I thought I was. Because you know, I had like this sense of you know, I have to be strong to deal with things like my life is really not that bad. And then when I was diagnosed, I was like, I felt relieved and significant in a way. Like I´m not crazy for feeling that way. ” (P09, 22, Female)
“No, um, because when I was diagnosed, initially, five years ago, um, I think I did at that point because it was just after I was diagnosed that I decided to study psychology. And I think before that, I was also under this impression of, ´Yeah it´s all just in your head, you should be strong´, and um, that kind of stuff. I think the internalized stigma I probably experienced at the beginning, like very beginning, but it was just a few months after I was diagnosed, that I started to realize that, ´Okay, this is real, this isn't just me being I don't know a little baby or whatever. ´ Actually having a diagnosis has taught me a lot. That´s something I wouldn´t have expected and yeah it had made me who I am essentially.” (P10, 25, Female)
Sub-theme: Getting out of the "depressed rut"—self-reliance, self-awareness, and dispositional optimism
Many participants credited their mental wellbeing to inborn or learned independence or confidence. Others mentioned gaining these attributes in early adulthood (for example, through life experiences). Participants described these attributes as helpful in that they were better able to ignore stigmatizing attitudes and beliefs around their mental health diagnoses. These participants had lower internalized stigma because they rejected social messages; they attributed this capacity to higher wellbeing.
Participants stressed the importance of maintaining a positive attitude in order to avoid becoming permanently depressed. Most participants expressed that having a set routine is helpful in gaining a sense of contentment, while being self-aware of the pre-stages of a “rut” can aid in an optimistic attitude. Some participants were able to implement a mindset of looking for happier life experiences despite their mental health conditions.
“For me the first step is, the easier you can cast it out of your mind, as a first step, the happier you will be already… Once you have that solidified, I think it is much easier to then think you know, ´There’s no reason for me to care what they think of me. There’s no reason for me to let that take up so much space in my mind. ´ And as a consequence of that, chances are you won’t be stigmatized as much because people will see that you're in more control.” (P21, 21, Male)
Theme three: Stigma fosters secrecy versus disclosure
Disclosure of mental illness was commonly identified as being based on the trust, understanding, support, and care given by the person they are sharing their feelings with. Some participants who were not always able to hide their conditions due to physical signs and symptoms (i.e., incisions and scars) found the idea of secrecy and/or lying difficult. Still, many who took part said that they do not talk about their mental conditions. Participants stated that keeping mental illnesses a “secret” was done to avoid potential frustration and disappointment from others’ lack of understanding and support. Participants suggested that talking about their mental illnesses would lead to more adverse outcomes (i.e., further misunderstanding and stigmatization), which would hurt rather than help their overall wellbeing.
“...sometimes I feel like I'm being a bit dishonest and like if I'm hiding something and it makes me feel bad if ‘m not being honest. But other times, it just makes me feel frustrated because I feel like I can’t tell them.” (P02, 21, Female)
“Generally, I will be open with people even if I don’t particularly want them to know because a lot of the time, I feel like I can’t hide it. I have like, visible scars on my arms. So, I feel like it’s really hard for people not to know most of the time, and so I sort of feel like, yeah, just be as open as I can.” (P03, 24, Female)
“By not talking about it [I feel protected] ...It means that most times, I can pretend that I don’t have a problem and can´t disappoint people counting on me…” (P15, 25, Female)
Sub-theme: Suffering in silence – the choice of secrecy
Participants described not wanting to share mental health details as a way to avoid feelings of weakness, incompetence, and insignificance. The majority of participants thought it would be ideal to suffer in silence rather than be a burden to others.
“I really don’t want to talk about it... I just feel like it’s something like I’d rather not acknowledge that I have. So, I’ll tell people, ´Oh no, I’m just having a bad day.´ But there are times where I would like to talk to people but I just cry myself to sleep alone and then wake up pretend everything is okay. I really don’t like talking about it. I can´t say for sure why. But maybe it’s because I don’t want people to judge me, but I don’t like talking about it at all. Not with anyone.” (P17, 22, Male)
Participants said that one way to avoid talking about mental health issues is to lie about them. This was also said: it is their first instinct to lie when trying to avoid the topic. Participants also talked about hiding medications or taking them in private. This was done so that no one else would ask questions that would lead to a conversation about mental health.
“...Also, I had to hide my antidepressants that I got from the doctor this year while I was taking them, because I don’t take them all the time, just when I’ve been prescribed. So, I thought I had to hide them to avoid people asking what´s wrong or why am I taking medication or something.” (P15, 25, Female)
Sub-theme: Seeking disclosure for freedom
Disclosure was recognized as a helpful part of expressing one’s thoughts and feelings—to those with whom participants trust, feel better understood, and feel unjudged. Participants gave numerous accounts of how they told others about their mental health problems because they thought it would help build trust, strengthen relationships, and give them more freedom.
“Um, it´s not as if you´re off-loading onto them, trying to give them the problem. You´re just being honest, which I guess is a good first step if you want to grow and be more mature for me anyway.” (P01, 21, Male)
“I feel like being open about mental health issues, um, just shows other people like, that’s okay... And they start to realize maybe there’s something I need to deal with... So, I think just talking about it and just breaking the stigma just helps people with, um, underlying disorders in general.” (P03, 24, Female)
Theme four: Stigma increases loneliness driven by avoidance of social contexts
Participants with depressive symptoms were asked to discuss how they manage social situations and the uncomfortable emotions that can arise when around other people. Many participants shared that in order to avoid these kinds of situations and, as a result, unpleasant emotions, they would prefer to be alone.
Sub-theme: Choosing to spend time alone
Some participants expressed feeling grateful to have time to themselves and said that they would like to be around other people if they did not have to deal with discrimination. The majority of the participants said they were aware that when they were alone and did not have any outside interactions or distractions, they may be inclined to reflect on negative thoughts and feelings.
“I prefer to spend time alone so that nobody will look down on me and nobody will stigmatize me. So, I prefer staying all alone…” (P13, 25, Male)
Sub-theme: Seeking alone time for purpose
Many participants identified time alone as a means to fulfill a number of purpose-oriented goals. This time alone allowed them to feel still and peaceful, revitalized and restored, and to reflect on their past week. As a result, they felt more confident in themselves. Further goals included doing simple activities they enjoyed (i.e., reading), making sense of things, or finding meaning in life.
“Often, I think when I look back and how my week went and how I spend my evenings, I definitely could have planned in a couple of times where I could have tried to see more people. That wouldn´t have affected me negatively at all. If anything, I would have made me feel a bit better. Take what I feel I´ve learned and put it into practice. Otherwise, you're just stagnating, and you get caught in the same cycle. I think you can make other people just as much a part of your life just as much as you make yourself. Like it's my choice, making my life just about me.” (P01, 21, Male)
“So sometimes I prefer to spend time with like my close-knit circle. Um, but I'm also very comfortable being alone. But um like I normally use my alone time for quite a bit of reflection, and yeah, I find this really helps, like it's good for my mental health.” (P07, 20, Other)
Sub-theme: The desire to socialize
Being around other people did not relieve feelings of isolation and aloneness, but in addition, participants shared that alone time did not help improve their mental health. The majority of participants expressed that being alone was not always their desired choice but rather a consequence of being mentally drained in social situations. For example, constantly worrying about what other people think of you and how they will react to or evaluate specific things you say or do. As a result, stigma may be exacerbated or introduced.
“It takes effort, I find, to talk to some people. And often it takes effort, mostly because of how critical I am of the way that I am talking. I am constantly thinking about what will be the best thing to say in this situation. What will they think of this if I say this, etc.? And that can be quite tiring, and I find that, especially with a lot of my friends who are quite introverted and have a social battery, you can see the exact moment when it runs out and they want to be alone, and um...You know what I mean? I mean, like… if I had the choice, it would be to be around my friends and to get out more. But yeah… So, it is hard to say that being on my own helps. It is just something that, at times, I need to. It´s more a consequence of being tired. And I think I am not going to be of any benefit to anyone if I talk to them in this state, so I am just going to relax and do my own thing. So that´s often the thought process behind being alone, I think.” (P01, 21, Male)
“So, I think that it definitely brings in that isolation factor of, like, you know, it's difficult to make friends because there's this constant voice in your head saying like, ´You're not worthy. People don't like you´, and like all of that. So then, you´re kind of, like, it's difficult to like make friends or make meaningful connections or like get out of your head enough to put yourself out there even though you really want to.” (P14, 21, Female)
For some, socializing is related to the desire to show others a “better” version of themselves, while others say they use socializing as an agent of distraction or numbness.
“Yeah, I think even if I’m talking with them happily and they think I am outgoing. But I think they don’t know me. Yeah, I’m still alone. Just, uh... It’s my mask or it’s my uh, uh, uh outside expression… Although like it might be false, at least I get to portray a better person...Specifically with depression, I’d say that you probably find life easier if you just try to fake it till you make it around other people. Whether that’s the right thing or not to do, you'll find life easier if you fake it till you make it.”.” (P19, 19, Male)
“I prefer to spend time with others because it’s sort of like a distraction and a numbing agent. I get to, like, I get to only portray the side of myself that makes me happy, I guess.” (P19, 19, Male)
That said, many participants were aware of the fact that socializing would be beneficial for their mental health despite existing stigmas, even if they did not necessarily feel like it.
“Uh, these experiences, uh, personally, makes me to really think this is much better to be alone rather than when we are with people even though this doesn´t benefit me. I, I want to be social. I want to be around my friends. Uh… but you know anything can still happen and you still get victimized or, because uh… you know when I am with people I forget about the depression. But I can’t do this if I get victimized you know… It´s hard. (P04, 25, Male)
There is a growing interest in developing evidence-based strategies to fight the impacts of stigma among depressed youths [ 32 ]. This qualitative study explored the subjective experiences associated with public and internalized stigma among young people with depression symptoms. It builds on the existing literature focusing primarily on deficits in knowledge about stigma and barriers to mental health care [ 32 , 38 , 50 ] and addresses the need for research on young people's subjective experiences of stigma and its effects on a number of emotional (e.g., loneliness) and functional (e.g., isolation) dimensions of their social relationships.
Our study suggested that mental health stigma continues to be a significant problem experienced by the younger population; most participant responses referred to having experienced externalized public stigma across their lifetimes. They felt judged, misunderstood, and insignificant. The vast majority of those described had internalized these stigmatizing experiences. Notably, the majority of participants described this process as occurring over time, stating that their experiences with stigma began in public and gradually became internalized.
We identified four main themes that reflected patterns in participant responses to interview questions, which highlighted that stigma’s negative effects on young people’s experiences of depression occur for varying reasons. Summarized in the first theme (titled Others’ Misunderstanding of Mental Health Disorders and the Impact Misunderstanding Has on Relationships ), the young people with depression with whom we talked often felt misunderstood (i.e., the lack of and/or lack of understanding of friends and family, the support system, the formation of bonds, and the strengthening or weakening of relationships) and stereotyped by others due to their MDD, resulting in fractured relationships. Effects of Stigma on the Self and Wellbeing (i.e., in the context of development, self-identity, wellbeing, and personality) reflected our observations that stigmatizing experiences harmed participants' self-identity, influencing their self-worth, self-esteem, and overall wellbeing in negative ways. Stigma Fosters Secrecy Versus Disclosure (i.e., mindset, circumstances, and experiences) recognized that participants discussed predictors that caused them to feel embarrassed about their depression, leading to views that secrecy is necessary and inhibiting disclosure. On the contrary, participants also identified reasons as to why some individuals disclose their mental illness, such as because it provides a way to find comfort and closure.
In our final theme, Stigma Increases Loneliness Driven by Avoidance of Social Context Bonds (i.e., loneliness, social isolation, and social circles) , we identified that stigma related to MDD is an isolating experience that affects communicating with others, socializing, the formation of bonds, and increases the desire to be alone. Most participants had negative stigma experiences, which in turn led them to choose to spend time alone even when alone time was not a valued activity. Being alone was a tool for managing stereotypical attitudes and beliefs and avoiding further stigmatizing experiences within the social context. That said, many actively anticipated, planned for, or sought periods of alone time as a way to find balance with their noisy, outer worlds.
Our findings that Others’ Misunderstanding of Mental Health Disorders and the Impact Misunderstanding Has on Relationships are aligned with previous studies with young people [ 9 , 16 , 103 ]. They highlight the relevance of stigma for driving feelings of being misunderstood and judged and build on a body of work that has largely focused on lack of parental warmth and support and childhood maltreatment as early predictors of MDD (i.e., parent–child relationships, lower positivity, negative emotionality, and disconstraint) [ 80 , 89 ]. Research has consistently shown that relationships between people and their effects on internal experiences shape development in complex ways and are likely to interact with one another to affect the onset of depression [ 80 , 90 ].
Research findings have shown how crucial it is to make social support networks safer (e.g., by focusing on improving mental health understanding in relationships) in order to reduce the risk of depression and potentially treat it during the developmental phase, when depressive symptoms usually start to appear and peak [ 16 , 43 ]. Interventions that emphasize supportive and understanding parent and peer relationships reduce depression symptoms [ 40 ]. In our sample, participants reported that their negative emotions (i.e., feelings of shame and guilt) deterred them from investing in relationships and taking part in social interactions where misunderstanding and stereotypes attached to depression are consequential factors. Such social interactions were seen to reflect a lack of understanding and interplayed with internal factors (i.e., effects on self-esteem, self-confidence, and insecurities) in determining whether young people with depression chose to invest time in these relationships.
Further reflecting on our theme, Effects of Stigma on the Self and Wellbeing , it is worth noting that stigma had an important influence on self-esteem and self-worth in our sample, an observation that echoes studies in young people [ 7 , 73 , 76 , 82 , 99 ]. Past research has also found links between experiences of mental health stigma and reduced wellbeing [ 28 ]. Our study showed that for many participants, having a formal diagnosis unintentionally changed the way one saw oneself (i.e., lowered self-confidence, self-esteem, and self-worth, as well as increased insecurities and a lack of identity). As a result of these self-processes, young people with depression were more likely to avoid social situations. They increased social withdrawal as a result of adverse self-views (i.e., poorer wellbeing).
It is worth noting that despite these costs, a few participants benefited from having a formal diagnosis, such as gaining unexpected insights and understanding the importance of one's mental health in accepting oneself (bringing about feelings of relief and recognition). This finding is consistent with past research, which has shown the importance of self in young people with depression [ 63 ].
Our findings that stigma fosters secrecy versus disclosure are in line with previous studies, which have found people keep their depression a secret because they feel ashamed. Furthermore, people with depression may be reluctant to acknowledge their illness due to the guilt and stigma associated with it [ 13 , 104 ]. Past studies have identified that secrecy can be a way to protect against stigma despite its adverse long-term consequences, such as loneliness and social isolation [ 75 ]. In line with previous research, our study showed that for many participants, talking about depression led to more adverse outcomes (i.e., added stigma, stereotypical attitudes and beliefs, and increased judgement), thus limiting their desire to disclose depression [ 15 ].
In addition, our findings that stigma increases loneliness driven by avoidance of social contexts have been found in both adults and youths [ 6 , 60 , 62 ]. Our participants described why they chose to spend time alone. Specifically, they highlighted isolation as a way to avoid stigma and discrimination. Alongside this avoidance goal, time alone held some benefits for young people. Many participants expressed having this time to fulfill purpose-oriented goals as well as for reflection, revitalization, restoration, and pleasureful activities, such as reading. Results further indicated participants' desires to socialize, even though this did not alleviate feelings of loneliness. This was often used as a way to show others a better version of themselves and is in line with past studies [ 2 , 98 ].
Given the importance that participants placed on feeling misunderstood or judged, it is important for practitioners who seek to help young people with depression to demonstrate understanding of mental health and stigma, as well as show empathy and care for depressed individuals' feelings and experiences. Doing so may have lasting positive impacts on wellbeing [ 16 ]. Through its findings, the current study extends the literature in several ways. While many studies have focused on stigma, our study explores young people's subjective experiences, an area in which research on the younger population is limited. Findings extend understanding of stigma effects, identifying their implications for feelings of loneliness, social isolation, and disrupted relationship experiences. Few studies, if any, have looked at all these ideas simultaneously in this population with an emphasis on depression.
Limitations and future directions
The qualitative study provided rich data and gave voice to young people with a formal diagnosis of depression and those who reported high symptoms of depression. However, we only recruited one in-patient participant, and therefore, it is possible that the more severe cases of MDD were not captured in this study. Furthermore, it was difficult to tell which aspects of the participants’ experiences were due to stigma itself and which were due to the nature of MDD impact on wellbeing. Future qualitative and quantitative research could examine depressive symptoms and stigma side-by-side to identify their unique and dependent effects on social and emotional wellbeing.
Likewise, while there was some diversity among participants in terms of socio-economic status and gender, the study would have benefited from greater diversity in terms of geography and culture, as this will be important as we continue to seek an understanding of mental health stigma. Mental health is understood and received differently in various countries, and as a result, stigma may have diverse consequences across cultures [ 64 ]. That said, this study was not designed or equipped to disentangle culture from individual participant experiences, but we sought diverse views that reflected participants’ unique experiences within their different cultures. Future quantitative research can rigorously examine the extent to which the subjective experiences described by the participants in this study are representative of those of the larger population of young people exhibiting depressive symptoms within their cultural context, but future qualitative research can also explore with participants how they see their particular sociocultural conditions affecting stigma and its outcomes.
Young people's accounts revealed a wide range of consequences beyond their depression diagnosis. Participants described stigma in relation to their depression in terms of often feeling discriminated against, misunderstood, and judged by others as a result of public stigma; they discussed internalizing these attitudes. They suggested that a lack of understanding from others, for example from their partners, family, and peers, and unreliable and/or absent support systems resulted in increased feelings of loneliness and social isolation, which reduced the quality and quantity of social relationships. Stigma also reduced their self-esteem and confidence, which in turn fostered secrecy and a reluctance to disclose their depression. The young people, however, also reported having long-term goals and aspirations to reconnect with others. These goals stood in contrast to feeling hopeless and unmotivated during periods of depression. Overall, we reveal how stigma can impact feelings of loneliness, social isolation, and relationships among young people with depression, which could lead to targeted interventions to lessen the impact of stigma in this population.
Acknowledgements
We would like to thank all participants who took part in helping us collect some of the data for this study.
Abbreviations
Major depressive disorder
Mood and Feelings Questionnaire
Thematic analysis
Authors’ contributions
KP, NW, and CM conceptualised and designed the present study. KP developed the interview questionnaire, conducted interviews, collected, transcribed, and analysed data with support from NW and CM. KP led the manuscript write-up and revisions in collaboration with NW and CM. All authors read and approved the final manuscript.
NW time on the project was funded by the European Research Council (ERC SOAR-851890). This project received no other funding.
Availability of data and materials
Study data are transcripts of interviews containing identifiable information. Data is not publicly available due to concerns that participant privacy may be compromised. Anonymised and de-identified data may be requested from the corresponding author.
Declarations
Ethics approval and consent to participate.
This study was conducted in accordance with the Declaration of Helsinki. The study was approved by the University Research Ethics Committee (2022–072-NW) of the University of Reading. Informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Katie Prizeman, Email: [email protected].
Netta Weinstein, Email: [email protected].
Ciara McCabe, Email: [email protected].
- 1. Achterbergh L, Pitman A, Birken M, Pearce E, Sno H, Johnson S. The experience of loneliness among young people with depression: a qualitative meta-synthesis of the literature. BMC Psychiatry. 2020;20(1):415. doi: 10.1186/s12888-020-02818-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Andrews B, Qian M, Valentine JD. Predicting depressive symptoms with a new measure of shame: The Experience of Shame Scale. Br J Clin Psychol. 2002;41(Pt 1):29–42. doi: 10.1348/014466502163778. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Austin JK, MacLeod J, Dunn DW, Shen J, Perkins SM. Measuring stigma in children with epilepsy and their parents: instrument development and testing. Epilepsy Behav. 2004;5(4):472–482. doi: 10.1016/j.yebeh.2004.04.008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54(1):37–44.e32. doi: 10.1016/j.jaac.2014.10.010. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Barbalat G, Plasse J, Gauthier E, Verdoux H, Quiles C, Dubreucq J, Legros-Lafarge E, Jaafari N, Massoubre C, Guillard-Bouhet N, Haesebaert F, Franck N. The central role of self-esteem in the quality of life of patients with mental disorders. Sci Rep. 2022;12(1):7852. doi: 10.1038/s41598-022-11655-1. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Barreto M, van Breen J, Victor C, Hammond C, Eccles A, Richins MT, Qualter P. Exploring the nature and variation of the stigma associated with loneliness. J Soc Pers Relat. 2022;39(9):2658–2679. doi: 10.1177/02654075221087190. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Christine Strlich. Depression: Causes and Treatment by Aaron T. Beck and Brad A. Alford, J Hosp Librarianship. 2010;10(3):326. 10.1080/15323269.2010.492268.
- 8. Ben-Zeev D, Young MA, Corrigan PW. DSM-V and the stigma of mental illness. J Ment Health. 2010;19(4):318–327. doi: 10.3109/09638237.2010.492484. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Brage D, Meredith W, Woodward J. Correlates of loneliness among midwestern adolescents. Adolescence. 1993;28(111):685–693. [ PubMed ] [ Google Scholar ]
- 10. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [ DOI ] [ Google Scholar ]
- 11. Brohan E, Elgie R, Sartorius N, Thornicroft G. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophr Res. 2010;122(1–3):232–238. doi: 10.1016/j.schres.2010.02.1065. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Buhs ES, Ladd GW, Herald SL. Peer exclusion and victimization: Processes that mediate the relation between peer group rejection and children's classroom engagement and achievement? J Educ Psychol. 2006;98:1–13. doi: 10.1037/0022-0663.98.1.1. [ DOI ] [ Google Scholar ]
- 13. Byrne P. Stigma of mental illness and ways of diminishing it. Adv Psychiatr Treat. 2000;6(1):65–72. doi: 10.1192/apt.6.1.65. [ DOI ] [ Google Scholar ]
- 14. Cacioppo JT, Patrick W. Loneliness: Human nature and the need for social connection. W W Norton & Co. 2008.
- 15. Camacho G, Reinka MA, Quinn DM. Disclosure and concealment of stigmatized identities. Curr Opin Psychol. 2020;31:28–32. doi: 10.1016/j.copsyc.2019.07.031. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Chirkov VI, Ryan RM. Parent and Teacher Autonomy-Support in Russian and U.S. Adolescents: Common Effects on Well-Being and Academic Motivation. J Cross-Cult Psychol. 2001;32(5):618–635. doi: 10.1177/0022022101032005006. [ DOI ] [ Google Scholar ]
- 17. Clayborne ZM, Varin M, Colman I. Systematic Review and Meta-Analysis: Adolescent Depression and Long-Term Psychosocial Outcomes. J Am Acad Child Adolesc Psychiatry. 2019;58(1):72–79. doi: 10.1016/j.jaac.2018.07.896. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, Anderson W, Dhansay MA, Phillips A, Shurin S, Walport M, Ewart W, Savill SJ, Bordin IA, Costello EJ, Durkin M, Fairburn C, Glass RI, Hall W, Huang Y, Hyman SE, Jamison K, Kaaya S, Kapur S, Kleinman A, Ogunniyi A, Otero-Ojeda A, Poo MM, Ravindranath V, Sahakian BJ, Saxena S, Singer PA, Stein DJ. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi: 10.1038/475027a. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Cooper K, Hards E, Moltrecht B, Reynolds S, Shum A, McElroy E, Loades M. Loneliness, social relationships, and mental health in adolescents during the COVID-19 pandemic. J Affect Disord. 2021;289:98–104. doi: 10.1016/j.jad.2021.04.016. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Corrigan PW, Kerr A, Knudsen L. The stigma of mental illness: Explanatory models and methods for change. Appl Prevent Psychol. 2005;11(3):179–190. doi: 10.1016/j.appsy.2005.07.001. [ DOI ] [ Google Scholar ]
- 21. Corrigan PW, Kerr AN, Knudsen L. The stigma of mental illness: Explanatory models and methods for change. Appl Prev Psychol. 2005;11:179–190. doi: 10.1016/j.appsy.2005.07.001. [ DOI ] [ Google Scholar ]
- 22. Corrigan PW, Larson JE, Rüsch N. Self-stigma and the "why try" effect: impact on life goals and evidence-based practices. World Psychiatry. 2009;8(2):75–81. doi: 10.1002/j.2051-5545.2009.tb00218.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Corrigan PW, Penn DL. Lessons from social psychology on discrediting psychiatric stigma. Stig Health. 2015;1:2–17. doi: 10.1037/2376-6972.1.S.2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16–20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Costello EJ, Angold A. Scales to assess child and adolescent depression: checklists, screens, and nets. J Am Acad Child Adolesc Psychiatry. 1988;27(6):726–737. doi: 10.1097/00004583-198811000-00011. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Crocker J, Major B, Steele C. Social Stigma. In: Gilbert DT, Fiske ST. and Lindzey G, Eds., The Handbook of Social Psychology, 4th Edition, Vol. 2. New York: Academic Press; 1998. p. 504-53.
- 27. Crosnoe R. Friendships in Childhood and Adolescence: The Life Course and New Directions. Soc Psychol Q. 2000;63:377. doi: 10.2307/2695847. [ DOI ] [ Google Scholar ]
- 28. Cruwys T, Gunaseelan S. “Depression is who I am”: Mental illness identity, stigma and wellbeing. J Affect Disord. 2016;189:36–42. doi: 10.1016/j.jad.2015.09.012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Daviss WB, Birmaher B, Melhem NA, Axelson DA, Michaels SM, Brent DA. Criterion validity of the Mood and Feelings Questionnaire for depressive episodes in clinic and non-clinic subjects. J Child Psychol Psychiatry. 2006;47(9):927–934. doi: 10.1111/j.1469-7610.2006.01646.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. de Jong Gierveld J, van Tilburg T, Dykstra P. Cambridge handbook of personal relationships. 2. 2018. Loneliness and social isolation: New ways of theorizing and conducting research; pp. 391–404. [ Google Scholar ]
- 31. DeFleur ML. Stigma: Notes on the Management of Spoiled Identity. By Erving Goffman. Englewood Cliffs, New Jersey: Prentice-Hall, 1963. 147 pp. Cloth, $4.50; paper, $1.95. Soc Forces. 1964;43(1):127–128. doi: 10.1093/sf/43.1.127. [ DOI ] [ Google Scholar ]
- 32. DeLuca JS. Conceptualizing Adolescent Mental Illness Stigma: Youth Stigma Development and Stigma Reduction Programs. Adolesc Res Rev. 2020;5(2):153–171. doi: 10.1007/s40894-018-0106-3. [ DOI ] [ Google Scholar ]
- 33. Dooley B, Fitzgerald A. My world survey: national study of youth mental health in Ireland. 2012. [ Google Scholar ]
- 34. Dumont M, Provost MA. Resilience in Adolescents: Protective Role of Social Support, Coping Strategies, Self-Esteem, and Social Activities on Experience of Stress and Depression. J Youth Adolesc. 1999;28(3):343–363. doi: 10.1023/A:1021637011732. [ DOI ] [ Google Scholar ]
- 35. Dunn V, Goodyer IM. Longitudinal investigation into childhood- and adolescence-onset depression: psychiatric outcome in early adulthood. Br J Psychiatry. 2006;188:216–222. doi: 10.1192/bjp.188.3.216. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Eigenhuis E, Waumans RC, Muntingh ADT, Westerman MJ, van Meijel M, Batelaan NM, van Balkom AJLM. Facilitating factors and barriers in help-seeking behaviour in adolescents and young adults with depressive symptoms: a qualitative study. PLoS One. 2021;16(3):e0247516. doi: 10.1371/journal.pone.0247516. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Eisenberg D, Downs MF, Golberstein E, Zivin K. Stigma and help seeking for mental health among college students. Med Care Res Rev. 2009;66(5):522–541. doi: 10.1177/1077558709335173. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Ferrie J, Miller H, Hunter SC. Psychosocial outcomes of mental illness stigma in children and adolescents: a mixed-methods systematic review. Child Youth Serv Rev. 2020;113:104961. doi: 10.1016/j.childyouth.2020.104961. [ DOI ] [ Google Scholar ]
- 39. Franko DL, Striegel-Moore RH, Thompson D, Schreiber GB, Daniels SR. Does adolescent depression predict obesity in black and white young adult women? Psychol Med. 2005;35(10):1505–1513. doi: 10.1017/s0033291705005386. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Gariépy G, Honkaniemi H, Quesnel-Vallée A. Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry. 2016;209(4):284–293. doi: 10.1192/bjp.bp.115.169094. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Ge L, Yap CW, Ong R, Heng BH. Social isolation, loneliness and their relationships with depressive symptoms: a population-based study. PLoS One. 2017;12(8):e0182145. doi: 10.1371/journal.pone.0182145. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Przyborski A, Wohlrab-Sahr M. Goffman, Erving: Stigma. In: Arnold, H.L. (eds) Kindlers Literatur Lexikon (KLL). J.B. Metzler, Stuttgart. 2020. 10.1007/978-3-476-05728-0_9208-1.
- 43. Goodman RJ, Samek DR, Wilson S, Iacono WG, McGue M. Close relationships and depression: a developmental cascade approach. Dev Psychopathol. 2019;31(4):1451–1465. doi: 10.1017/s0954579418001037. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Guba EG, Lincoln YS. Competing paradigms in qualitative research. 1994. [ Google Scholar ]
- 45. Guest G, McLellan E. Distinguishing the Trees from the Forest: Applying Cluster Analysis to Thematic Qualitative Data. Field Methods. 2003;15(2):186–201. doi: 10.1177/1525822X03015002005. [ DOI ] [ Google Scholar ]
- 46. Guest G, Namey E, Chen M. A simple method to assess and report thematic saturation in qualitative research. PLoS One. 2020;15(5):e0232076. doi: 10.1371/journal.pone.0232076. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Oyebode J. Qualitative Research Methods in Mental Health and Psychotherapy: A Guide for Students and Practitioners Edited by David Harper & Andrew R. Thompson. Wiley-Blackwell. 2011. £29.99 (pb). 272 pp. ISBN: 978-0470663707. The British Journal of Psychiatry. 2012;200(5):435–435. 10.1192/bjp.bp.112.108746.
- 48. Hawton K, Saunders KE, O'Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379(9834):2373–2382. doi: 10.1016/s0140-6736(12)60322-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Hay DF, Payne A, Chadwick A. Peer relations in childhood. J Child Psychol Psychiatry. 2004;45(1):84–108. doi: 10.1046/j.0021-9630.2003.00308.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Heary C, Hennessy E, Swords L, Corrigan PW. Stigma towards Mental Health Problems during Childhood and Adolescence: Theory, Research and Intervention Approaches. J Child Fam Stud. 2017;26:2949–2959. doi: 10.1007/s10826-017-0829-y. [ DOI ] [ Google Scholar ]
- 51. Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353–363. doi: 10.1080/13548500600595327. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Hertzman C, Boyce T. How experience gets under the skin to create gradients in developmental health. Annu Rev Public Health. 2010;31:329–347 323p following 347. doi: 10.1146/annurev.publhealth.012809.103538. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Hinshaw SP. The stigmatization of mental illness in children and parents: developmental issues, family concerns, and research needs. J Child Psychol Psychiatry. 2005:46(7). 10.1111/j.1469-7610.2005.01456.x. [ DOI ] [ PubMed ]
- 54. Hinshaw SP, Stier A. Stigma as related to mental disorders. Annu Rev Clin Psychol. 2008;4:367–393. doi: 10.1146/annurev.clinpsy.4.022007.141245. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Huggett C. A qualitative study exploring experiences of stigma by people with mental health problems. 2016. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Johnco C, Rapee RM. Depression literacy and stigma influence how parents perceive and respond to adolescent depressive symptoms. J Affect Disord. 2018;241:599–607. doi: 10.1016/j.jad.2018.08.062. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Josephson JR, Josephson SG. Abductive inference: computation, philosophy, technology. 1994. Cambridge University Press.
- 58. Kakilla C. Strengths and Weaknesses of Semi-Structured Interviews in Qualitative Research: A Critical Essay. 2021. [ Google Scholar ]
- 59. Kaushik A, Kostaki E, Kyriakopoulos M. The Stigma of Mental Illness in Children & Adolescents: A Systematic Review [Article] Psychiatry Res. 2016 doi: 10.1016/j.psychres.2016.04.042. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Kerr NA, Stanley TB. Revisiting the social stigma of loneliness. Pers Individ Differ. 2021;171:110482. doi: 10.1016/j.paid.2020.110482. [ DOI ] [ Google Scholar ]
- 61. Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60(7):709–717. doi: 10.1001/archpsyc.60.7.709. [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. Kong L, Gao Z, Xu N, Shao S, Ma H, He Q, Zhang D, Xu H, Qu H. The relation between self-stigma and loneliness in visually impaired college students: Self-acceptance as mediator. Disabil Health J. 2021;14(2):101054. doi: 10.1016/j.dhjo.2020.101054. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Korrelboom K, Maarsingh M, Huijbrechts I. Competitive memory training (COMET) for treating low self-esteem in patients with depressive disorders: a randomized clinical trial. Depress Anxiety. 2012;29(2):102–110. doi: 10.1002/da.20921. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Krendl AC, Pescosolido BA. Countries and Cultural Differences in the Stigma of Mental Illness: The East-West Divide. J Cross Cult Psychol. 2020;51(2):149–167. doi: 10.1177/0022022119901297. [ DOI ] [ Google Scholar ]
- 65. Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev. 2016;69:313–332. doi: 10.1016/j.neubiorev.2016.07.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Lovett L, Tamkin A, Fletcher J. Children's Views on Mental Illness. Int J Health Promot Educ. 2011;49(1):4–8. doi: 10.1080/14635240.2011.10708200. [ DOI ] [ Google Scholar ]
- 68. Mathew AR, Pettit JW, Lewinsohn PM, Seeley JR, Roberts RE. Co-morbidity between major depressive disorder and anxiety disorders: shared etiology or direct causation? Psychol Med. 2011;41(10):2023–2034. doi: 10.1017/s0033291711000407. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 69. Matthews T, Danese A, Caspi A, Fisher HL, Goldman-Mellor S, Kepa A, Moffitt TE, Odgers CL, Arseneault L. Lonely young adults in modern Britain: findings from an epidemiological cohort study. Psychol Med. 2019;49(2):268–277. doi: 10.1017/s0033291718000788. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Matthews T, Danese A, Wertz J, Odgers CL, Ambler A, Moffitt TE, Arseneault L. Social isolation, loneliness and depression in young adulthood: a behavioural genetic analysis. Soc Psychiatry Psychiatr Epidemiol. 2016;51(3):339–348. doi: 10.1007/s00127-016-1178-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 71. Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 72. Mikami AY, Normand S. The Importance of Social Contextual Factors in Peer Relationships of Children with ADHD. Curr Dev Disord Rep. 2015;2(1):30–37. doi: 10.1007/s40474-014-0036-0. [ DOI ] [ Google Scholar ]
- 73. Morgades-Bamba CI, Fuster-Ruizdeapodaca MJ, Molero F. The impact of stigma on subjective well-being in people with mental disorders. Clin Schizophr Relat Psychoses. 2017 doi: 10.3371/csrp.Cbmf.071317. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. Mukolo A, Heflinger CA, Wallston KA. The stigma of childhood mental disorders: a conceptual framework. J Am Acad Child Adolesc Psychiatry. 2010;49(2):92–103; quiz 198. doi: 10.1097/00004583-201002000-00003. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 75. Mulfinger N, Rüsch N, Bayha P, Müller S, Böge I, Sakar V, Krumm S. Secrecy versus disclosure of mental illness among adolescents: I. The perspective of adolescents with mental illness. J Ment Health. 2019;28(3):296–303. doi: 10.1080/09638237.2018.1487535. [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Orth U, Robins RW, Roberts BW. Low self-esteem prospectively predicts depression in adolescence and young adulthood. J Pers Soc Psychol. 2008;95(3):695–708. doi: 10.1037/0022-3514.95.3.695. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Paskaleva-Yankova A. Interpersonal and Intersubjective Alienation in Social Stigmatization and Depression. Psychopathology. 2022;55(3):201–210. doi: 10.1159/000519253. [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed., Thousand Oaks: Sage; 2002.
- 79. Patton MQ. Qualitative Research. In Encyclopedia of Statistics in Behavioral Science. 2005 doi: 10.1002/0470013192.bsa514. [ DOI ] [ Google Scholar ]
- 80. Pfeiffer PN, Heisler M, Piette JD, Rogers MA, Valenstein M. Efficacy of peer support interventions for depression: a meta-analysis. Gen Hosp Psychiatry. 2011;33(1):29–36. doi: 10.1016/j.genhosppsych.2010.10.002. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 81. Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–365. doi: 10.1111/jcpp.12381. [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. Ranøyen I, Stenseng F, Klöckner CA, Wallander J, Jozefiak T. Familial aggregation of anxiety and depression in the community: the role of adolescents' self-esteem and physical activity level (the HUNT Study) BMC Public Health. 2015;15:78. doi: 10.1186/s12889-015-1431-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 83. Rhew I, Simpson K, Tracy M, Lymp J, McCauley E, Tsuang D, Vander Stoep A. Criterion validity of the Short Mood and Feelings Questionnaire and one- and two-item depression screens in young adolescents. Child Adolesc Psychiatry Ment Health. 2010;4:8. doi: 10.1186/1753-2000-4-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 84. Rose AL, Atkey SK, Goldberg JO. Self-Stigma in Youth: Prevention, Intervention, and the Relevance for Schools. 2018. [ Google Scholar ]
- 85. Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. Eur Psychiatry. 2005;20(8):529–539. doi: 10.1016/j.eurpsy.2005.04.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Salaheddin K, Mason B. Identifying barriers to mental health help-seeking among young adults in the UK: a cross-sectional survey. Br J Gen Pract. 2016;66(651):e686–692. doi: 10.3399/bjgp16X687313. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. 2018;2(3):223–228. doi: 10.1016/s2352-4642(18)30022-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 88. Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, Angermeyer MC. Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand. 2012;125(6):440–452. doi: 10.1111/j.1600-0447.2012.01826.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 89. Shannon A, Flett GL, Goldberg JO. Feelings of Not Mattering, Perceived Stigmatization for Seeking Help, and Help-Seeking Attitudes among University Students. Int J Ment Heal Addict. 2020;18(5):1294–1303. doi: 10.1007/s11469-019-00138-6. [ DOI ] [ Google Scholar ]
- 90. Solantaus T, Paavonen EJ, Toikka S, Punamäki RL. Preventive interventions in families with parental depression: children's psychosocial symptoms and prosocial behaviour. Eur Child Adolesc Psychiatry. 2010;19(12):883–892. doi: 10.1007/s00787-010-0135-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 91. Steinberg L. Cognitive and affective development in adolescence. Trends Cogn Sci. 2005;9(2):69–74. doi: 10.1016/j.tics.2004.12.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 92. Sund A, Larsson B, Wichstrøm L. Prevalence and characteristics of depressive disorders in early adolescents in central Norway. Child Adolesc Psychiatry Ment Health. 2011;5:28. doi: 10.1186/1753-2000-5-28. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 93. Świtaj P, Grygiel P, Anczewska M, Wciórka J. Loneliness mediates the relationship between internalised stigma and depression among patients with psychotic disorders. Int J Soc Psychiatry. 2014;60(8):733–740. doi: 10.1177/0020764013513442. [ DOI ] [ PubMed ] [ Google Scholar ]
- 94. Swords L, Hennessy E, Heary C. Qualitative methods advancing research into the expression and experience of stigma in childhood and adolescence. Stigma and Health. 2021;6:20–26. doi: 10.1037/sah0000286. [ DOI ] [ Google Scholar ]
- 95. Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379(9820):1056–1067. doi: 10.1016/s0140-6736(11)60871-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 96. Thornicroft G, Sunkel C, AlikhonAliev A, Baker S, Brohan E, El Chammay R, Davies K, Demissie M, Duncan J, Fekadu W, Gronholm PC, Guerrero Z, Gurung D, Habtamu K, Hanlon C, Heim E, Henderson C, Hijazi Z, Hoffman C, Hosny N, Huang FX, Kline S, Kohrt BA, Lempp H, Li J, London E, Ma N, Mak WWS, Makhmud A, Maulik PK, Milenova M, Morales Cano G, Ouali U, Parry S, Rangaswamy T, Rüsch N, Sabri T, Sartorius N, Schulze M, Stuart H, Taylor Salisbury T, Vera San Juan N, Votruba N, Winkler P. The Lancet Commission on ending stigma and discrimination in mental health. Lancet. 2022;400(10361):1438–1480. doi: 10.1016/s0140-6736(22)01470-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 97. Tuckett AG. Applying thematic analysis theory to practice: a researcher’s experience. Contemp Nurse. 2005;19(1–2):75–87. doi: 10.5172/conu.19.1-2.75. [ DOI ] [ PubMed ] [ Google Scholar ]
- 98. Velotti P, Garofalo C, Bottazzi F, Caretti V. Faces of Shame: Implications for Self-Esteem, Emotion Regulation, Aggression, and Well-Being. J Psychol. 2017;151(2):171–184. doi: 10.1080/00223980.2016.1248809. [ DOI ] [ PubMed ] [ Google Scholar ]
- 99. Wehmeier PM, Schacht A, Barkley RA. Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. J Adolesc Health. 2010;46(3):209–217. doi: 10.1016/j.jadohealth.2009.09.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 100. WHO . Adolescent Mental Health Fact Sheet. 2020. [ Google Scholar ]
- 101. WHO. The World health report: 2003: Adolescent mental health. World Health Organization; 2023. https://www.who.int/news-room/factsheets/detail/adolescent-mental-health .
- 102. Wicks D. The Coding Manual for Qualitative Researchers (3rd edition)The Coding Manual for Qualitative Researchers (3rd edition) Johnny Saldaña Sage 2015 ISBN-13: 978-1473902497. Qual Res Organ Manag. 2017;12:169–170. doi: 10.1108/QROM-08-2016-1408. [ DOI ] [ Google Scholar ]
- 103. Wilson S, Vaidyanathan U, Miller MB, McGue M, Iacono WG. Premorbid risk factors for major depressive disorder: are they associated with early onset and recurrent course? Dev Psychopathol. 2014;26(4 Pt 2):1477–1493. doi: 10.1017/s0954579414001151. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 104. Wolpert L. Stigma of depression – a personal view. Br Med Bull. 2001;57(1):221–224. doi: 10.1093/bmb/57.1.221. [ DOI ] [ PubMed ] [ Google Scholar ]
- 105. Wood A, Kroll L, Moore A, Harrington R. Properties of the Mood and Feelings Questionnaire in Adolescent Psychiatric Outpatients: A Research Note. J Child Psychol Psychiatry. 1995;36(2):327–334. doi: 10.1111/j.1469-7610.1995.tb01828.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2007;64(7):1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
- View on publisher site
- PDF (1018.8 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Research article
- Open access
- Published: 05 October 2018
A qualitative study on the stigma experienced by people with mental health problems and epilepsy in the Philippines
- Chika Tanaka ORCID: orcid.org/0000-0002-6288-5532 1 ,
- Maria Teresa Reyes Tuliao 2 ,
- Eizaburo Tanaka 3 ,
- Tadashi Yamashita 4 &
- Hiroya Matsuo 1
BMC Psychiatry volume 18 , Article number: 325 ( 2018 ) Cite this article
148k Accesses
37 Citations
8 Altmetric
Metrics details
Stigma towards people with mental health problems (PMHP) is known to have substantial negative impacts on their lives. More in-depth exploration of the stigma and discrimination experienced by PMHP in low- and middle-income countries is needed. Previous research suggests that negative attitudes towards PMHP are widespread among the Filipino general public. However, no study has investigated PMHP’s own experiences of being stigmatised in the Philippines.
A qualitative study was conducted on the stigma experienced by PMHP (including people with epilepsy) and its related factors in the Philippines, employing the constructivist grounded theory approach. We analysed data on 39 PMHP collected through interviews with PMHP, their carers, and community health volunteers who know them well.
The findings highlight the culturally and socio-economically specific contexts, consequences, and impact modifiers of experiences of stigma. Participants emphasised that PMHP face stigma because of the cultural traits such as the perception of mental health problem as a disease of the family and the tendency to be overly optimistic about the severity of the mental health problem and its impact on their life. Further, stigma was experienced under conditions where mental health care was not readily available and people in the local community could not resolve the PMHP’s mental health crisis. Stigma experiences reduced social networks and opportunities for PMHP, threatened the economic survival of their entire family, and exacerbated their mental health problems. An individual’s reaction to negative experiences can be fatalistic in nature (e.g. believing in it is God’s will). This fatalism can help PMHP to remain hopeful. In addition, traditional communal unity alleviated some of the social exclusion associated with stigma.
Conclusions
The study indicates that existing stigma-reduction strategies might have limitations in their effectiveness across cultural settings. Therefore, we propose context-specific practical implications (e.g. emphasis on environmental factors as a cause of mental health problems, messages to increase understanding not only of the possibility of recovery but also of challenges PMHP face) for the Philippines.
Peer Review reports
Stigma and discrimination against people with mental health problems (PMHP) are a global public health issue [ 1 , 2 , 3 ] and can have substantial negative impacts on all aspects of a person’s life, from employment and housing to social and family life [ 4 , 5 , 6 , 7 ]. Public stigma, the general public’s reaction towards a stigmatised group, can be conceptualised as having three distinct elements [ 8 ]. First, a negative belief about a stigmatised group is seen as stereotype. Second, an emotional reaction to the stereotype is seen as prejudice. Third, a behavioural manifestation of the prejudice is discrimination. Historically, research on stigma related to mental health has been conducted mainly on stereotypes, prejudices, and intentions to discriminate that are held by the general public with regard to PMHP. Such research revealed that the general public frequently label PMHP as dangerous, blameworthy, incompetent and weak, which is often accompanied with emotions of fear and anger and can lead to behavioural intention of avoidance, punishment, and coercion [ 9 , 10 , 11 , 12 ]. Further, the literature shows that internalisation of public stigma or self-stigma is also frequent among PMHP, which reduces self-esteem, causes social isolation, and inhibits help-seeking behaviour [ 6 , 13 , 14 , 15 ].
Recent research has more often investigated levels of discrimination using direct reports from PMHP. The results of such research suggest that discrimination against PMHP is a universal phenomenon around the world [ 2 , 3 , 16 ]; however, PMHP’s experiences of discrimination and its related factors might differ in high-income countries (HICs) versus low- and middle- income countries (LMICs). Some studies suggest that PMHP experience a lower level of stigma in LMICs [ 17 ], such as India [ 18 ], China [ 19 ], and Nigeria [ 20 ], compared with HICs. The reasons for the more positive acceptance of PMHP in those settings have been considered to be a more supportive environment with social cohesion as well as more social role options that PMHP are able to fulfil [ 21 , 22 ]. At the same time, there is also accumulating evidence revealing that in LMICs, experiences of stigma, discrimination and human rights abuses related to mental health problems are common and severe [ 23 , 24 , 25 , 26 , 27 ]. The stigmatisation in LMICs has been attributed to the combined effects of socioeconomic and ethno-cultural characteristics of the setting [ 28 ]. For example, the economic situation of widespread poverty may contribute to further marginalisation of PMHP who are not able to financially contribute to society [ 29 ]. Moreover, the cultural value of collectivism may results in discrimination towards PMHP especially with regarding to marriage and childrearing, since a person’s mental health problem is often seen as the family’s mental health problem [ 30 ]. Overall, practices and outcomes of stigma differ across cultures and socioeconomic backgrounds [ 29 , 31 , 32 ], and meaningful comparison across cultural settings may not be achievable with cross-cultural measures [ 33 ]. In consideration of this, researchers have called for an in-depth qualitative exploration of the experiences of stigma among PMHP in LMICs settings, where about 85% of the world’s population live [ 21 ].
PMHP in the Philippines, a lower-middle income country in Asia, might experience a significant level of stigma and discrimination. Filipino immigrants believed that personal characteristics (i.e. self-centeredness and “soul weakness”) resulted in mental health problems [ 34 , 35 ], which have been shown to be related to blaming PMHP and discriminatory behaviour in other settings [ 36 ]. Also, a multi-country survey revealed that, among 16 countries surveyed, the Philippines had the second highest proportion of citizens who agreed that PMHP should not be hired for a job even if they are qualified [ 37 ]. Further, some studies that involved interviews with Filipino immigrants living in Australia and the United States and that sampled from the general population revealed that a fear of being labelled as ‘crazy’ and spoiling their family’s reputation made Filipinos hesitate to seek help from mental health professionals [ 35 , 38 , 39 ]. Although these previous studies provide some knowledge regarding public stigma in the Filipino context, all of them looked at stereotypes, prejudices and intentions to discriminate held by the general public towards PMHP. To our knowledge, there is no study investigating PMHP’s own experiences of being stigmatised and discriminated against and the related factors in the Philippines.
To fill the gaps in the literature, we conducted a qualitative study on the factors related to experiences of stigma as well as the experiences itself of PMHP in the Philippines, using interviews with PMHP and people who know them well. Revealing the existence, types, and sources of stigma experienced by PMHP in the Philippines can contribute to the stigma research in Asian LMIC settings. Further, exploring the experiences of stigma and its related factors can provide fundamental knowledge for the design of an effective stigma reduction program in the Filipino setting.
The current research utilised the principles of constructivist grounded theory, which is deemed suitable for revealing the social phenomenon of PMHP’s experiences of stigma [ 40 ] in the Filipino context. The constructivist grounded theory assumes a relativist ontology (accepting that multiple realities exist) and a subjectivist epistemology (involving a co-construction of meaning through interaction between the researcher and participant) [ 41 ]. It provides a means of studying power, inequality, and marginality [ 42 ].
Our study was conducted in Muntinlupa, the southernmost city in the Philippines’ National Capital Region. The city has a population of 481,461 as of 2016. The majority comprises Tagalog ethnic groups and professes Christian, primarily Roman Catholic, faith. Households below the food threshold, the minimum income required to meet basic food needs, account for 21.5% of the total in the city [ 43 ]. The majority of citizens cannot afford private medical services, which cost five times more than the public medical services [ 44 ]. With respect to public psychiatric service, the city has one outpatient and no in-patient facility. The nearest public in-patient psychiatric facility is located about 23 km away.
Main data collection
Participants.
We collected data on PMHP from three different sources of information: PMHP themselves, their carers, and community health volunteers who knew them well. The eligibility criteria for PMHP were 1) having a mental health problem, listed in the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5), or epilepsy, and 2) currently not using residential care. Epilepsy was included for several reasons. First, people with epilepsy are known to suffer stigma and discrimination [ 45 , 46 ]. Second, the condition has a long history of being classified as a psychiatric problem [ 47 ]. Third, even with the present-day efforts promoting mental health in LMICs, epilepsy is often treated together with mental health issues [ 48 ]. Last, pilot interviews revealed that local lay people do not clearly differentiate epilepsy from mental health problems.
For the recruitment, we approached 42 PMHP in person; one of them declined to participate owing to time constraints. Thus, we obtained informed consent from 41 PMHP. Among them, two PMHP were excluded because they were confirmed to have only physical health problems and no mental health problems as listed in DSM-5. Consequently, we used data of 39 PMHP for our analysis. The profiles of the final sample are shown in Table 1 . In 20 of the PMHP, we interviewed the PMHP and their main carer, usually a parent or sibling. In the remaining 19 PMHP, only a main carer was interviewed, as the 19 PMHP had communication difficulties that hindered them from answering interview questions. Additionally, in 11 PMHP, we conducted interviews with a community health volunteer who was in charge of the district in which the PMHP lived.

Recruitment
We aimed to include a wide variation in the characteristics of the PMHP, namely, gender, age, marital status, educational attainment, employment status, religion, type of mental health problem, and history of using health and welfare services. To achieve this, the participants were recruited by purposive sampling in cooperation with two different collaborating stakeholders. First, as stigma was considered to inhibit Filipino people from seeking professional help for their mental condition [ 35 , 49 ], we recruited the majority of PMHP ( n = 36) in cooperation with community health volunteers, which enabled us to recruit PMHP regardless of their history of receiving health care. The community health volunteers had good knowledge of the profiles of the residents of the district under their charge and covered all the areas of the city. Second, we recruited a small number of PMHP ( n = 3) with common mental health problems (e.g. anxiety and depressive problems) from the outpatient clinical practice of a psychiatrist, as the community health volunteers did not identify any people with these types of problems.
To check the eligibility of those who had never been diagnosed by a specialist as having a mental health problem, a research member, ET, carefully reviewed the data of the individual participants, including interview recordings, transcriptions, and field notes, and then provided informed presumption if the participants had a mental health problem or not. ET also assessed which chapter, the broadest classification in DSM-5, the participant most fitted. ET has clinical experience as a psychiatrist in Japan for over 15 years.
Interview procedures
Data on the PMHP were collected through semi-structured in-depth interviews. Prior to the beginning of data collection, an interview guide was developed, referring to previous research [ 18 , 50 ], and then modified based on six pilot interviews in the setting. The interview guide had a series of open questions on three major topics: onset of mental health problems and coping behaviours, experiences of being treated negatively owing to the problem and its consequences, and activities PMHP gave up because of how others might respond to their health problem. The interview guides for interviews with PMHP and for interviews with carers and community health volunteers can be accessed in Additional files 1 and 2 , respectively. Consistent with the grounded theory methods, we used the interview guide as a flexible tool that could be revised as the analysis progressed. The carers and community health volunteers were not asked about their own experiences of stigma as a carer or person working in mental health. Instead, we asked them about the PMHP’s experiences regarding the same topics, based on their observations. Demographic data of the PMHP were also obtained at the beginning of the interview.
The first author, CT (female, a Japanese public health nurse), conducted all of the data collection between January and March 2017. During the interview, Tagalog or English was used as preferred by the participants. When Tagalog was chosen, the interviews were interpreted by one of two health workers who had lived in the city for more than 30 years and were fluent in both Tagalog and English. After explaining the study and gaining informed consent, the interviews were conducted in their home, a health centre, or the city hospital, depending on the participants’ preference. Wherever possible, we conducted interviews in a space where there was no one but the interviewee, interviewer, and interpreter around. However, five PMHP were not willing to be interviewed alone. In which case, a family member was in the same place and assisted the interview. All the interviews were digitally recorded with interviewees’ permission and lasted between 19 and 53 min; the median length was 29 min. The participants received 100 Philippine pesos (1.9 US dollars) as acknowledgement for their participation.
Supplementary data collection
We included data of interviews with seven health workers into our analysis to gain a wider perspective on the stigma experienced by PMHP. CT conducted the interviews during her one-month participant observation at health services provided by the city government. During the observation, CT discussed the role of stigma and its impact on PMHP with more than 85 health and welfare workers. We analysed seven interviews with those who shared episodes on PMHP with whom they were in direct contact as a part of their duty at work. The interviewees were three community health volunteers, two nurses, one doctor, and one rehabilitation program officer. Notes were taken during the interviews and six out of seven interviews were audiotaped with their permission.
All of the recordings were transcribed verbatim by two trained transcribers. Tagalog recordings were simultaneously translated into English by the transcribers fluent in English and Tagalog. An independent research assistant randomly selected 10% of the English transcripts and checked their accuracy by matching them with the Tagalog and English recordings. During this checking process, no significant errors were found thus the transcripts were quality assured.
Data analysis started as soon as the initial data were collected. We set aside theoretical ideas from the existing literature; instead, we remained open to exploring the theoretical possibilities we could discern from the data. After reading each of the transcripts at least twice, CT and ET independently conducted the initial coding. Simple codes were created to describe the phenomenon in each segment of data, using the qualitative data analysis software, Nvivo Version 11.4.1 (QSR International, 2016). The initial codes with identical meanings were merged through discussion, whereas those with different meanings were left unchanged to increase the variety in the interpretation of the data. We used data from interviews with cares, health volunteers, health and welfare workers to increase variety of data on stigma experienced by PMHP and gain comprehensive understanding of its context. Thus, when accounts showed some discrepancy between a person with mental health problem and his/her carer or a person who knew him/her well, we used the data from both accounts for our analysis.
The authors gradually moved on to the focus coding, in which the initial codes were concentrated on or collapsed into categories that make analytical sense, and then tested these against extensive data. The interpersonal interaction between people with and without mental health problems was treated as the central phenomenon of our interest. To explore comprehensively PMHP’s experiences of stigma, we decided to treat any “uncomfortable treatments from others” reported as stigma experience, regardless of the actors’ motivation. We constantly compared data on similarities and differences within a participant as well as across participants to examine the categories and develop links among them. CT led the preliminary focus coding. Subsequently, discussions were held between CT, ET, and HM, in which we reviewed the developed categories and links to determine if they were grounded in data and sufficiently explained the phenomenon.
After analysing the data of the 35 PMHP, a tentative model that explains the relations between categories was developed. We then collected and analysed data on four additional PMHP. Through discussion, the full research team determined that the categories and themes were sufficiently relevant and that the model held true for these additional PMHP. We then concluded that the model was theoretically saturated.
Analyses revealed four interrelated themes surrounding stigma experienced by PMHP: (1) the context affecting stigma experience, (2) stigma experience, (3) impact modifier of the stigma experience, and (4) consequence of the stigma experience. Figure 1 shows the relationship among the themes.
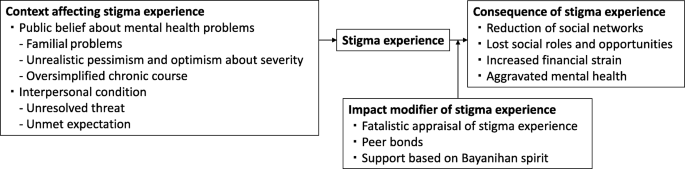
Stigma experienced by people with mental health problems and its related factors in the Philippines
Context affecting stigma experience
We identified two contextual categories that changed how others treated PMHP in a negative way.
Public belief about mental health problems
Public beliefs surrounding mental health issues are a contextual category of stigma experienced by PMHP in the Philippines. It consists of three themes: familial problems, unrealistic pessimism and optimism about severity, and oversimplified chronic course.
Familial problems
Community health volunteers and health workers observed that families of PMHP and people in the local community do not provide appropriate support for PMHP because they perceive mental affliction as a family problem and indicative of so-called “bad blood”. The belief that mental health problems can be transmitted among relatives pushed families of PMHP to deny the existence of mental health issues and people in the community to distance themselves from PMHP. A nurse shared an episode of a male patient with depression:
His family could not accept the idea that one of their relatives is actually depressed. (…) It’s because in our culture, when it comes to mental illness, it tends to be a family affair. People think if one of you has a history of mental illness, there is a chance that almost all of you already have that as well. We care about how others think about our family more than anything else. And other people feel that it is not their place to intervene in some family matters. (Interview 48, Nurse, Female)
In particular, marrying age PMHP faced stigma because of the belief in heredity. People in the community often believe that PMHP have mental health problems in their family’s blood and are afraid of developing those problems in their kinship via marriage.
I had one neighbour that I reported to the barangay [district government] because she mocked me. She was saying that I had mental illness in our blood and no one dare marry me and get in trouble. (Interview 51, PMHP, Male)
Unrealistic pessimism and optimism about severity
PMHP experienced stigma when others were overly pessimistic about the severity of a mental health problem. Participants often criticised those who believe that mental health problems generally cause severe functional impairments. This belief has resulted in unfair treatment towards PMHP in the Philippines.
[Researcher: What is the biggest challenge for the [social inclusion] program?] Finding a job. It’s very difficult. The community people don’t believe they [PMHP] are functional and don’t hire them. (…) So now some barangays [district governments] have started to hire them. We hope people see them working hard and start to trust them. (Interview 27, Rehabilitation program officer, Male)
Meanwhile, unrealistic optimism about its severity also caused stigma. The commonly held belief is that individuals are able to overcome any psychological suffering by themselves, and as a result, it will not become a serious problem. It was common for PMHP to be doubted or withheld empathy in such a culture that emphasises resilience and humour under stressful situations.
Filipinos are proud of being resilient. We find something funny in any difficult situation. But when you have this illness, that kind of thinking gives you a huge pressure. (…) One day, I opened up about my mental illness to my friends, but they all had the same reaction. They laughed at me and didn’t take it seriously. (Interview 71, PMHP, Female)
Oversimplified chronic course
The oversimplified chronic course of mental health problems emerged as one of the causes of stigma. People without any experience of a mental health problem often misunderstand the repetitive relapse and remission in the course of a mental health problem. They tend to apply an acute illness model and expect a complete cure in the short term. However, as the symptoms are prolonged, they begin to mistrust the PMHP’s account.
After one month of no work, I was able to work and sleep. But in February, it came back. I couldn’t sleep for several days. (...) My supervisors were thinking that I should be working a night shift duty, but I told them that I would have to take sick leave. But because it was the same reason for my previous absent, they are already thinking that I am making up stories. (Interview 30, PMHP, Male)
Interpersonal condition
Interpersonal condition was identified as a direct trigger of stigma experience. It consists of two themes: unresolved threat and unmet expectation.
Unresolved threat
Unresolved threat is a condition where PMHP are at risk of hurting themselves or others owing to their mental health problems, with the people in contact with the PMHP failing to manage such risks. Under such conditions, PMHP often experience physical violence, being avoided, and being restricted by others. Although the PMHP, their families, and community health volunteers attributed the threats to PMHP’s personal factors, such as personality and outwardly noticeable symptoms, they also emphasised the culpability of people in the local community for their lack of understanding and skills in interacting with PMHP. When others became familiar with PMHP, they successfully managed those threats and prevented PMHP from experiencing stigma. The mother of a boy with a neurodevelopmental problem told us:
My son easily becomes violent. For example, when someone takes and plays with his toy. The neighbours don’t understand why he is angry and they bully him. But there are also some playmates who fully understand him. When they know that my son is about to be angry, they immediately keep distance from him. And after a while, my son calms down and they start playing around together. (Interview 4, Mother of a boy with a mental health problem)
Unmet expectation
Unmet expectation was another context of stigma. In this context, there is a gap between PMHP’s abilities and other people’s expectations of them. Some PMHP reported suffering from stigma when others’ expectations were too high for their situation. People in this cultural setting tend to value strong bonds and reciprocity among families and neighbours. PMHP sometimes were unable to perform in accordance with this value owing to their mental health conditions. Violation of this value was judged as morally wrong.
They [the neighbours] say I should help my mum by doing washing, cleaning, and taking care of my brother, even when I say I feel weak or don’t know how to. (Interview 5, PMHP, Female) She is big but still doesn’t help her mother. That’s why the neighbours don’t like her. They say she is not a good daughter. (Interview 18, Community health volunteer, Female)
Meanwhile, some other PMHP experienced stigma when others underestimated PMHP’s abilities. Families often criticised other people that looked only at PMHP’s disabilities but not at their abilities.
When someone in our neighbourhood was trying to talk to my sister and she did not respond back, they started bullying her and calling her crazy. [Researcher: How do you think we can change such situation?] I think proper communication towards her would be the best since she’s really a good listener. The problem is that other people don’t know she actually understands things really well. (Interview 8, Sister of a woman with a mental health problem)
Stigma experience
Although we frequently found that PMHP were positively treated by others because of their mental health problems, we also discovered that almost all the PMHP participants were faced with negative treatment from others. PMHP experienced psychological abuse (e.g. being verbally insulted, laughed at, stared at, gossiped about, doubted), physical violence (e.g. being hit, stones being thrown at them), being restricted (e.g. being told not to go outside alone, tied with a rope to a pillar), not being supported (e.g. lack of understanding and sympathy), being taken advantage of (e.g. being cheated out of money and belongings), being neglected (e.g. privacy not being protected, medical care not being provided), and being rejected (e.g. not being associated with, not being hired). Families were an important source of stigma in terms of prominence as stigma from families was often repetitive (e.g. frequently being slapped) and prolonged (e.g. being locked up in a room for several months). PMHP also experienced stigma frequently from their neighbours, and sometimes from school friends, co-workers and employers. People who were involved with PMHP as a part of their duty at work (i.e. health workers and public safety officers) were a source of stigma as well. For complete information on the stigma experience by source, please see Table 2 .
Impact modifier of stigma experience
Even if the nature of stigma experiences were similar, the extent and degree of its influence on PMHP’s life varied depending on impact modifier of stigma experience . PMHP had three impact modifiers consisting of internal (i.e. fatalistic appraisal) and external (i.e. peer bonds, community unity) factors.
Fatalistic appraisal of stigma experience
Fatalistic appraisal of stigma experience offered PMHP and their families a strategy to cope with the emotional pain caused by stigma experience. People in the setting generally believed that God predetermined life events in the past, present and future. Some PMHP and their family accepted unfair treatments from others as “fate.” They were able to remain hopeful because they believed that God would help them if they had faith in God.
Sometimes people say he is crazy. [Researcher: What do you do in response to that?] Nothing. People say what they want to say. We just say “God is good.” As long as we believe in Him, it will be alright. (Interview 23, Sister of a man with a mental health problem)
Peer bonds , the emotional bonds with other people with similar mental health problems, empowered PMHP to change their stigmatised situation in a positive way. Stigma experience could marginalise them in the community, but when they were together with peers who understood not only their health condition but also their lowered social status, they were empowered and motivated to change the situation for themselves and their peers.
[Researcher: What are the barriers to your recovery?] The different perceptions of people towards us [she and other people with mental health problems]. It is so discouraging for us. And we are the only ones who can understand each other very well. We are like brothers and sisters already. Nevertheless, we make sure that the reason we join the [rehabilitation] program is not only for ourselves but to show them that we can change ourselves for the better. If we will be given a chance to work again, we will make 100 percent effort to get things done accordingly. (Interview 34, PMHP, Female)
Support based on Bayanihan spirit
Support based on Bayanihan spirit , a traditional concept of community unity, relieved the negative impacts of stigma on PMHP. It was not rare that community people gave food or rented a house free to PMHP and their family who had little income. Helping one another in a time of need was inherent in their lives, called Bayanihan in Tagalog. For example, a homeless woman with schizophrenia told us that she had felt hopeless because she had been bullied at school and was in a materially deprived circumstance. However, she was now enjoying her life and managing to make a living because some of her neighbours treated her as a valued community member (e.g. regularly invited her to a local dancing event) and occasionally gave her food. A community health volunteer explained why she had good relationships with the community as follows:
That is natural here. When your family member is sick, neighbours and friends are there to pay for medicines, bring food, help with housework, and take care of small kids. We call it Bayanihan. (Interview 3, Community health volunteer, Female)
Consequence of stigma experience
Stigma experience was found to bring about a substantial negative impact on PMHP’s social networks, roles, opportunities, and mental health.
Reduction of social networks
Stigma experience reduced PMHP’s social networks, which led to them spending their days isolated at home without any interaction with people outside of their immediate family. This was due not only to the direct influence of experiences of stigma (i.e. being physically restrained , being avoided by others ) but also the indirect influence of changes in three aspects: PMHP’s behaviour, restriction by families, and relationships with others. First, after being negatively treated, PMHP tended to “close off to everybody” and distanced themselves from others.
Going out is sometimes like an obstacle. (…) After that [hearing my friends gossiping about me], I have been afraid of people’s judgments. (Interview 62, PMHP, Female)
Second, families started to restrict PMHP’s behaviour to protect them from further stigma experiences.
We do not allow him to go out. We are afraid that something like that [neighbours calling him crazy] might happen to him again or someone might abduct him. (Interview 9, Sister of a man with a mental health problem)
Third, stigma experiences provoked conflicts, from a quarrel to a physical fight, and worsened the relationship between PMHP and others. The conflicting relationships produced a further stigmatising attitude towards PMHP.
He got into a fight with his playmates because they said bad words to him. (…) Many of our neighbours told me that he should be in a cell. They told me that they knew a policeman who could put him in jail. (Interview 1, Mother of a man with metal health problem)
Lost social roles and opportunities
As a result of stigma experience, PMHP lost social roles and opportunities , such as being employed, going to school, having a romantic partner, getting married, parenting, helping with household chores and the family business, taking care of younger siblings and joining religious activities.
She was a member of the choir in church. She likes singing and has a good voice. And plenty of friends visited her in the past and they went to church together. But no more. Nobody visits her, and she quit attending it. (Interview 10, Mother of a woman with a mental health problem)
Increased financial strain
Lost social roles and opportunities increased financial strain, which negatively affected the families as well as PMHP themselves. In this setting, PMHP and their families lived in communities where many people find it difficult to make a living. The cost of transportation to medical facilities and treatment fees put them in a further difficult situation economically. In such conditions, entire families often suffered from the financial strain that was due to stigma to the degree that they could not afford basic items including food and clothing.
If only I could find a good job like when I was well. Even though we do not have enough money to buy things, my family really makes an effort to find ways that we can buy those medicines. (Interview 20, PMHP, Male)
Aggravated mental health
The participants reported that the stigma experiences aggravated mental health in PMHP. The memory of negative treatment from others often stuck in their mind and its influence lasted for a long time. A 32-year-old woman with anxiety problem explained how the experience of being bullied when she was a teenager influenced her current condition:
It triggers my anxiety. When I remember their facial expressions, even now, I feel overwhelmed and breathless (Interview 39, PMHP, Female).
The experience of stigma also affected the mental health condition of PMHP by preventing them from seeking help. Some PMHP and their families choose to keep their mental health status a secret. However, families have limited capacities to take care of a person with a mental health problem, especially in the case of someone with severe symptoms. In the worst case in terms of the influence of stigma on PMHP’s mental health, a community health volunteer reported that the parents of a daughter with a mental health problem locked her up in her room and took care of her without seeking professional help. However, her condition kept deteriorating and eventually she committed suicide inside her room.
To our knowledge, this is the first study to document the stigma experienced by PMHP in the Philippines. This study adds to the understanding of discrimination in LMIC settings and its related contextual factors in the Philippines.
First, our results showed that PMHP in the Philippines experienced stigma, which brought about negative impacts on PMHP’s social networks, roles and opportunities, financial burden, and mental health. Although stigma types, sources, and areas of impact were generally consistent with the existing literature in this field [ 4 , 6 , 51 ], we found that experiences of stigma threatened the economic survival of the entire family of PMHP and increased the mental health crisis in the LMIC context, given the minimal welfare and mental health care provisions. Several studies with participants recruited from clinical settings have shown that PMHP in LMICs suffered less from stigma [ 2 , 18 , 19 , 20 ]. In this study, we involved PMHP without psychiatric service use, which prevented us from overlooking the stigma experienced by the poorest and most marginalised PMHP. Our findings might better reflect the reality in LMIC settings, where it is estimated that more than 70% of PMHP receive no treatment for their mental health conditions [ 52 ].
Second, we found that pessimistic and over-optimistic reactions to a mental health problem are among the important contexts of experiences of stigma in the Philippines. Historically, stigma research has mainly focused on the pessimistic view on the prognosis and its negative effects [ 10 , 53 , 54 , 55 , 56 ]. Meanwhile, when the over-optimistic view on the outcome of mental health problems has been documented among Filipino immigrants, it was only recognised as a barrier to help-seeking [ 35 , 39 ]. Our qualitative exploration’s original finding is that the over-optimistic belief among the community regarding the severity of mental health problems results in PMHP’s receiving inappropriate or negative treatment. This is an important finding for the Philippines, because resilience and optimism under difficult situations are among the well-known cultural traits of Filipinos [ 57 , 58 ]. Stigma resulting from optimism might be prevalent in the Philippines; a prior study showed that among the 16 countries, the Philippines posted the highest proportion of respondents who agreed that mental illness would improve on its own [ 59 ].
Third, the results indicated that mental health problems were perceived as problems of the family and discouraged people from accepting mental health problems. The finding is consistent with psychiatrists’ clinical experiences with Filipino patients [ 60 , 61 ]. We also found that a belief in transmissibility among relatives led to PMHP experiencing reduced marriage opportunities. Previous studies conducted on Chinese descent groups [ 62 , 63 , 64 ] showed that the threat of genetic contamination was related to endorsement of reproductive restriction. We propose that it might hold true in the Filipino context, meaning that the threat to family lineage through genetic contamination via marriage accounts for some of the discrimination experienced by PMHP.
Fourth, we revealed a context-specific impact modifier of stigma experiences, namely, fatalistic appraisal of stigma experience . Existing studies have discussed that Filipinos typically attribute illness to “the will of God” [ 39 , 49 , 65 ]. A new finding of this study is that negative treatments from others were also attributed to fate. Globally, it is known that fatalistic appraisal of negative events inhibits active coping and worsens health [ 66 , 67 ]. However, we found that fatalism offered a spiritual coping strategy and shielded PMHP from the adverse effects of stigma in the Catholic dominant setting of the Philippines. These findings are consistent with the literature that have showed that fatalism facilitates adjustment to negative life events [ 49 , 68 , 69 ]. Moreover, support based on Bayanihan spirit was another culturally relevant impact modifier. The origin of the Bayanihan spirit is traced back to the country’s tradition wherein towns’ people cooperate to carry a family’s entire house on their shoulders to a new location. It is considered a core essence of the Filipino culture. Our finding supports the arguments by Lasalvia [ 21 ] and Mascayano et al. [ 29 ] that communal network, which tends to be better maintained in LMICs, is among the existing strengths to reduce the negative effects of stigma.
Lastly, the research method of obtaining perspectives from multiple participants who witnessed and experienced stigma allowed us to reveal that the interpersonal conditions (i.e. unresolved threat and unmet expectations ) preceded stigma experiences. Consistent with previous research from India [ 24 ] and Indonesia [ 70 ], in the setting where mental health care is not readily available at a local level, people in the community needed to cope with the possible danger of PMHP to self or others and can violate PMHP’s human rights. Similar to the results of prior qualitative analyses of interviews with PMHP and their families [ 18 , 71 ], the expectations of others in contrast to PMHP’s actual capabilities caused negative reactions from others. Those interpersonal conditions might be a more important determinant of stigma experiences than PMHP’s personal factors, considering the previous studies showing individual variables (e.g. employment status, symptom, and treatment experiences) accounted for only less than 30% of total variance of experienced stigma [ 2 , 3 ].
Practical implications
Our results suggest that mental health care must have the objective of the reduction of stigma towards PMHP. The Department of Health and Local Government Units are required by the Mental Health Act [ 72 ], established in 2018 as the first law of its kind in the Philippines, to initiate and sustain nationwide campaigns to raise the level of awareness on the protection and promotion of mental health and rights. In conducting stigma reduction campaigns, they should: 1) target families of PMHP, community people, health workers, and public safety officers; 2) avoid genetic explanations for mental health problems and emphasise the role of environmental and social factors as its cause; 3) increase public understanding of not only the possibility of recovery but also the challenges that PMHP face; and 4) improve families’ and community members’ skills in assessing and coping with possible danger posed by PMHP to self or others [ 73 , 74 , 75 , 76 ]. These interventions might be more effective when they utilise the existing communal network and increase social contact between PMHP and others [ 77 , 78 ] We also propose that mental health and welfare services for PMHP should: 1) be community-based and support PMHP in meeting expectations that are meaningful for themselves and others; 2) provide opportunities for PMHP to share their experiences with peers to empower them [ 79 , 80 , 81 ]; and 3) prevent PMHP from internalising experiences of stigma with acknowledgement of fatalistic appraisal of them as a coping strategy. Lastly, to mitigate the adverse influences of stigma, it is necessary to change the structure of health care and welfare service provision for PMHP (e.g. inclusive education, welfare benefits, and job schemes). It is also essential to provide effective and accessible mental health care.
Study limitations
We were unable to recruit people with common mental health problems who were not using psychiatric services. In fact, community health volunteers do not recognise any people having common mental health problems. This may reflect stigma-related situations where local people do not recognise the manifestation of symptoms of those problems as a health issue, or where people with those problems hide their conditions. Additionally, cultural and language barriers may have played a part in data collection and interpretation. However, we also encountered a number of situations where the interviewee provided the data collector, who was from another cultural background, with further explanations, especially on their culture. Further, some interviews were too short to be considered an in-depth interview. Also, we needed to rely in part on data from narratives of people who know PMHP well, instead of from PMHP themselves. These were because the interviewer had difficulty encouraging some participants, especially PMHP, to talk about sensitive topics. Thus, there might be experiences and related themes that we could not explore. Lastly, we conducted the study in one city; thus, the results may not be generalisable to another part of the Philippines (e.g. rural and Muslim-dominant areas).
Our findings highlight that PMHP in the Philippines experience substantial discrimination and its adverse effects are severe to the degree that it threatens the financial survival of the entire family. Culture-bound beliefs and social structure (e.g. perceiving mental health problems as a familial problems, traditional communal unity) played important roles in shaping and modifying stigma experiences. More research is needed to develop stigma reduction interventions utilising these findings and to evaluate their effectiveness.
Abbreviations
The Diagnostic and Statistical Manual of Mental Disorders
High-income countries
Low- and middle-income countries
People with mental health problems
Seeman N, Tang S, Brown AD, Ing A. World survey of mental illness stigma. J Affect Disord. 2016;190:115–121. Available from: https://doi.org/10.1016/j.jad.2015.10.011 Elsevier.
Article Google Scholar
Lasalvia A, Zoppei S, Van Bortel T, Bonetto C, Cristofalo D, Wahlbeck K, et al. Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: a cross-sectional survey. Lancet. 2013;381:55–62. Available from: https://doi.org/10.1016/S0140-6736(12)61379-8 Elsevier Ltd
Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet; 2009;373:408–415. Available from: https://doi.org/10.1016/S0140-6736(08)61817-6 . Elsevier Ltd
Sharac J, McCrone P, Clement S, Thornicroft G. The economic impact of mental health stigma and discrimination: a systematic review. Epidemiol Psichiatr Soc. 2010;19:223. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21261218 .
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45:11–27 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24569086 .
Article CAS Google Scholar
Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71:2150–2161. Available from: https://doi.org/10.1016/j.socscimed.2010.09.030 Elsevier Ltd
Link BG, Phelan JC. Conceptualising stigma. Annu Rev Sociol. 2001 [cited 2018 Jul 3];27:363–385. Available from: https://www.annualreviews.org/doi/pdf/10.1146/annurev.soc.27.1.363
Corrigan PW. Mental health stigma as social attribution: implications for research methods and attitude change. Clin Psychol Sci Pract. 2006;7:48–67 Available from: http://doi.wiley.com/10.1093/clipsy.7.1.48 .
Mannarini S, Boffo M. Anxiety, bulimia, drug and alcohol addiction, depression, and schizophrenia: what do you think about their aetiology, dangerousness, social distance, and treatment? A latent class analysis approach. Soc Psychiatry Psychiatr Epidemiol. 2015;50:27–37.
McGinty EE, Goldman HH, Pescosolido B, Barry CL. Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Soc Sci Med; 2015;126:73–85. Available from: https://doi.org/10.1016/j.socscimed.2014.12.010 . Elsevier Ltd
Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113:163–79.
Corrigan PW, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44:162–79.
Corrigan P, Watson A. The paradox of self-stigma and mental illness. Clin Psychol Sci Pract. 2002;9:35–53 Available from: https://onlinelibrary.wiley.com/doi/10.1093/clipsy.9.1.35 .
Google Scholar
Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol Med. 2012;42:1741–52.
Mccann TV, Renzaho A, Mugavin J, Lubman DI. Stigma of mental illness and substance misuse in sub-Saharan African migrants: a qualitative study. Int J Ment Health Nurs. 2017;27:956–65.
Camden Schizoph E, Corker EA, Beldie A, Brain C, Jakovljevic M, Jarema M, et al. Experience of stigma and discrimination reported by people experiencing the first episode of schizophrenia and those with a first episode of depression: The FEDORA project Anamaria Vasilache 2 , Margda Waern 3,4 , Norman Sartorius 10 , Graham Thornicroft 1 and the FEDORA study group. Int J Soc Psychiatry. 2015 [cited 2018 Jul 3];61:438–445. Available from: http://journals.sagepub.com/doi/pdf/10.1177/0020764014551941
Lasalvia A, Van Bortel T, Bonetto C, Jayaram G, Van Weeghel J, Zoppei S, et al. Cross-national variations in reported discrimination among people treated for major depression worldwide : the ASPEN / INDIGO international study. Br J Psychiatry. 2015;207:507–14.
Koschorke M, Padmavati R, Kumar S, Cohen A, Weiss HA, Chatterjee S, et al. Experiences of stigma and discrimination of people with schizophrenia in India. Soc Sci Med; 2014;123:149–159. Available from: https://doi.org/10.1016/j.socscimed.2014.10.035 . Elsevier Ltd
Lv Y, Wolf A, Wang X. Experienced stigma and self-stigma in Chinese patients with schizophrenia. Gen Hosp Psychiatry. 2013;35:83–8. Available from: https://doi.org/10.1016/j.genhosppsych.2012.07.007 Elsevier Inc.
Oshodi YO, Abdulmalik J, Ola B, James BO, Bonetto C, Cristofalo D, et al. Pattern of experienced and anticipated discrimination among people with depression in Nigeria: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2014;49:259–66.
Lasalvia A. Tackling the mental illness stigma in low- and middle-income countries: lessons learned from high-income countries and mistakes to avoid. Epidemiol Psychiatr Sci. 2015;24:395–8 Available from: https://www.cambridge.org/core/journals/epidemiology-and-psychiatric-sciences/article/tackling-the-mental-illness-stigma-in-low-and-middleincome-countries-lessonslearned-from-highincome-countries-and-mistakes-to-avoid/83D63EA7FD15A3A3F2F9085E7E1700A2 .
Rosen A. Destigmatizing day-to-day practices: what developed countries can learn from developing countries. World Psychiatry. 2006;5:21–24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1472257/ .
Alonso J, Buron A, Bruffaerts R, He Y, Posada-Villa J, Lepine JP, et al. Association of perceived stigma and mood and anxiety disorders: results from the world mental health surveys. Acta Psychiatr Scand. 2008;118:305–14.
Mathias K, Kermode M, San Sebastian M, Koschorke M, Goicolea I. Under the banyan tree--exclusion and inclusion of people with mental disorders in rural North India. BMC Public Health. 2015;15:–446 Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-1778-2 .
Maramis A, Van Tuan N, Minas H. Mental health in Southeast Asia. Lancet. 2011;377:700–2.
Minas H, Diatri H. Pasung: Physical restraint and confinement of the mentally ill in the community. Int J Ment Health Syst. 2008;2 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2442049/ .
Tawiah PE, Adongo PB, Aikins M. Mental Health-Related Stigma and Discrimination in Ghana: Experience of Patients and Their Caregivers. Ghana Med J. 2015 [cited 2018 Jul 3];49:30–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26339082 .
Lauber C, Rössler W. Stigma towards people with mental illness in developing countries in Asia. Int Rev Psychiatry [Internet]. 2007;19:157–78 Available from: https://www.ncbi.nlm.nih.gov/pubmed/17464793 .
Mascayano F, Armijo JE, Yang LH. Addressing stigma relating to mental illness in low- and middle-income countries. Front Psychiatry. 2015;6:1–4.
Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms. Clin Psychol Rev. 2011;31:934–48.
Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L, Thornicroft G. stugma and discrimination related to mental illness in low- and middle-income countries. Epidemiol. Psychiatr. Sci. [Internet]. 2015;24:382–94. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25937022 .
Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2007;64:1524–35.
Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing “what matters most” to identify culture-specific aspects of stigma. Int. J. Epidemiol. [internet]. 2014;43:494–510. Available from. https://www.ncbi.nlm.nih.gov/pubmed/24639447 .
Edman JL, Johnson RC. Filipino American and Caucasian American beliefs about the causes and treatment of mental problems. Cultur Divers Ethnic Minor Psychol. 1999;5:380–6.
Thompson S, Hartel G, Manderson L, Woelz-Stirling N, Kelaher M. The mental health status of Filipinas in Queensland. Aust N Z J Psychiatry. 2002;36:674–80.
Corrigan PW, Rowan D, Green A, Lundin R, River P, Uphoff-Wasowski K, et al. Challenging two mental illness Stigmas : personal responsibility and dangerousness. Schizophr Bull. 2002;28:293–310.
Pescosolido BA, Medina TR, Martin JK, Long JS. The “Backbone” of Stigma: Identifying the Global Core of Public Prejudice Associated With Mental Illness. Am. J. Public Health [Internet]. 2013;103:853–60. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23488508 .
Gong F, Gage SJL, Tacata LA. Helpseeking behavior among Filipino Americans: a cultural analysis of face and language. J Community Psychol. 2003;31:469–88.
Javier JR, Supan J, Lansang A, Beyer W, Kubicek K, Palinkas LA. Preventing Filipino mental health disparities: perspectives from adolescents, caregivers, providers, and advocates. Asian Am J Psychol [Internet]. 2014;5:316–24 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4319658/ .
Charmaz K. Constructing Grounded Theory. 2nd ed. SAGE Publications Ltd; 2014.
Charmaz K. Grounded theory methods in social justice research. In: Denzin NK, Lincoln YS, editors. SAGE Handb. Qual. Res. SAGE; 2011. p. 359–380.
Charmaz K. The Power of Constructivist Grounded Theory for Critical Inquiry. Qual. Inq. [Internet]. 2017;23:34–45. Available from: http://journals.sagepub.com/doi/10.1177/1077800416657105
City Government of Muntinlupa. POVERTY AND EMPLOYMENT STATISTICS [Internet]. 2017 [cited 2017 Jun 30].
Philippine Statistics Authority. Philippines National Demographic and Health Survey 2013. 2013 [cited 2017 Jun 30]. Available from: https://dhsprogram.com/pubs/pdf/FR294/FR294.pdf .
Boling W, Means M, Fletcher A. Quality of Life and Stigma in Epilepsy, Perspectives from Selected Regions of Asia and Sub-Saharan Africa. Brain Sci. [Internet]. Multidisciplinary Digital Publishing Institute (MDPI); 2018 [cited 2018 Jun 27];8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29614761 .
Herrmann LK, Welter E, Berg AT, Perzynski AT, Van Doren JR, Sajatovic M. Epilepsy misconceptions and stigma reduction: Current status in Western countries. Epilepsy Behav. [Internet]. 2016 [cited 2018 Jun 27];60:165–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27208826 .
Koch-Stoecker S. Neuropsychiatric issues in epilepsy. In: Matsuura M, Inoue Y, editors. Neuropsychiatr. issues epilepsy [Internet]. John Libbey Eurotext; 2010 [cited 2018 Jun 27]. p. 233. Available from: https://books.google.co.jp/books?id=FQXhAAAAQBAJ&pg=PA174&lpg=PA174&dq=epilepsy+Emil+Kraepelin&source=bl&ots=r35Oh0rwjA&sig=IZa-67-5hrTVkzSl4HEIoGkaobQ&hl=en&sa=X&ved=0ahUKEwjd26SwkvPbAhWEnZQKHUvrDZsQ6AEIsAEwEw#v=onepage&q=epilepsyAQ28EmilKraepelin&f=false .
World Health Organization. mhGAP Training Manuals - for the mhGAP Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings, version 2.0 [Internet]. WHO. World Health Organization; 2017 [cited 2018 Jun 27]. Available from: http://www.who.int/mental_health/mhgap/training_manuals/en/
Tuliao AP. Mental health help seeking among Filipinos: a review of the literature. Asia Pacific J Couns Psychother [Internet]. 2014;5:124–36 Available from: http://www.tandfonline.com/doi/abs/10.1080/21507686.2014.913641 .
Yang LH, Valencia E, Alvarado R, Link B, Huynh N, Nguyen K, et al. A theoretical and empirical framework for constructing culture-specific stigma instruments for Chile. Cad. saude coletiva [Internet]. 2013;21:71–9. Available from: /pmc/articles/PMC3753780/?report=abstract.
Hamilton S, Pinfold V, Cotney J, Couperthwaite L, Matthews J, Barret K, et al. Qualitative analysis of mental health service users’ reported experiences of discrimination. Acta Psychiatr Scand. 2016;134:14–22.
Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA [internet]. 2004;291:2581–90. Available from. http://www.ncbi.nlm.nih.gov/pubmed/15173149 .
Wig NN, Suleiman MA, Routledge R, Murthy RS, Ladrido-Ignacio L, Ibrahim HH, et al. Community reactions to mental disorders. A key informant study in three developing countries. Acta Psychiatr. Scand. [Internet]. 1980;61:111–26. Available from: https://www.ncbi.nlm.nih.gov/pubmed/7361584 .
Ando S, Yamaguchi S, Aoki Y, Thornicroft G. Review of mental-health-related stigma in Japan. Psychiatry Clin Neurosci. 2013;67:471–82.
van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Comparing stigmatising attitudes towards people with substance use disorders between the general public, GPs, mental health and addiction specialists and clients. Int J Soc Psychiatry [Internet]. 2014;61:539–49 Available from: http://isp.sagepub.com/cgi/doi/10.1177/0020764014562051 .
Clement S, Jarrett M, Henderson C, Thornicroft G. Messages to use in population-level campaigns to reduce mental health-related stigma: consensus development study. Epidemiol Psichiatr Soc. 2010;19:72–9.
Dy MB. Values in Philippine culture and education. Washington, DC: CRVP; 1994.
Social Weather Stations. Social Weather Station Survey. [Internet]. 2017 [cited 2017 Nov 9]. Available from: https://www.sws.org.ph/swsmain/artcldisppage/?artcsyscode=ART-20170816103037
Pescosolido BA, Martin JK, Olafsdottir S, Long JS, Medina TR, Martin JK. The theory of industrial society and cultural schemata: does the “cultural myth of stigma” underlie the WHO schizophrenia paradox? Am J Sociol. 2015;121:783–825.
Araneta EG. Psychiatric Care of Pilipino Americans. In: Gaw AC, editor. Cult. Ethn. Ment. Illn. Washington, DC: American Psychiatric Press; 1993. p. 377–412.
Sanchez F, Gaw A. Mental health Care of Filipino Americans. Psychiatr Serv [Internet] 2007;58:810–815. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17535941
Wonpat-Borja AJ, Yang LH, Link BG, Phelan JC. Eugenics, genetics, and mental illness stigma in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol. 2012;47:145–56.
Yang LH, Purdie-Vaughns V, Kotabe H, Link BG, Saw A, Wong G, et al. Culture, threat, and mental illness stigma: identifying culture-specific threat among Chinese-American groups. Soc. Sci. Med. [internet]. Elsevier Ltd. 2013;88:56–67 Available from: https://doi.org/10.1016/j.socscimed.2013.03.036 .
Yang LH, Kleinman A. “Face” and the embodiment of stigma in China: the cases of schizophrenia and AIDS. Soc Sci Med. 2008;67:398–408.
Abad PJB, Tan ML, Baluyot MMP, Villa AQ, Talapian GL, Reyes ME, et al. Cultural beliefs on disease causation in the Philippines: challenge and implications in genetic counseling. J Community Genet. 2014;5:399–407.
De Los Monteros KE, Gallo LC. The relevance of fatalism in the study of Latinas’ cancer screening behavior: a systematic review of the literature. Int J Behav Med. 2011;18:310–8.
Roberts RE, Roberts CR, Chen IG. Fatalism and risk of adolescent depression. Psychiatry [internet]. 2000;63:239–52. Available from. http://www.ncbi.nlm.nih.gov/pubmed/11125670 .
Cheng H, Sit JWH, Twinn SF, Cheng KKF, Thorne S. Coping with breast Cancer survivorship in Chinese women the role of fatalism or fatalistic voluntarism. Cancer Nurs. 2013;36:236–44.
Gonzalez P, Nuñez A, Wang-Letzkus M, Lim J-W, Flores KF, Nápoles AM. Coping with breast cancer: reflections from Chinese American, Korean American, and Mexican American women. Heal Psychol [Internet] 2016;35:19–28. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26389720 .
Nurjannah I ,Mills J PT& UK. Human rights of the mentally ill in Indonesia. Int Nurs Rev. 2015;62:153–61.
Habtamu K, Alem A, Hanlon C. Conceptualizing and contextualizing functioning in people with severe mental disorders in rural Ethiopia: a qualitative study. BMC psychiatry [internet]. 2015;15:34. Available from: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-015-0418-9 .
An act establishing a national mental health policy for the purpose of enhancing the delivery of integrated mental health services, promoting and protecting the rights of persons utilizing psychiatric, neurologic and psychosocial health services, APPROPRI [Internet]. Republic of the Philippines; 2018. Available from: http://www.officialgazette.gov.ph/2018/06/20/republic-act-no-11036/
Kitchener B, Jorm A. Mental health first aid training for the public: evaluation of effects on knowledge, attitudes and helping behavior. BMC Psychiatry [Internet]. 2002;2:10. Available from: http://www.biomedcentral.com/1471-244X/2/10
Morgan AJ, Ross A, Reavley NJ. Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. Doran CM, editor. PLoS One [Internet]. 2018 [cited 2018 Jun 28];13:e0197102. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197102 .
Bond KS, Jorm AF, Kitchener BA, Reavley NJ. Mental health first aid training for Australian medical and nursing students: an evaluation study. BMC Psychol. [Internet]. 2015 [cited 2018 Jun 28];3:11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25914827 .
Jorm AF, Kitchener BA, Fischer J-A, Cvetkovski S. Mental Health First Aid Training by e-Learning: A Randomized Controlled Trial. Aust. New Zeal. J. Psychiatry [Internet]. 2010 [cited 2018 Jun 28];44:1072–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21070103 .
Corrigan PW, Morris SB, Michaels PJ, Rafacz JDRN. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr. Serv. [Internet]. 2012;63:963–73 Available from: https://www.ncbi.nlm.nih.gov/pubmed/23032675 .
Corrigan PW, Michaels PJ, Vega E, Gause M, Larson J, Krzyzanowski R, et al. Key ingredients to contact-based stigma change: A cross-validation. Psychiatr. Rehabil. J. [Internet]. 2014 [cited 2018 Jun 28];37:62–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24417232 .
Corrigan PW, Larson JE, Michaels PJ, Buchholz BA, Del Rossi R, Fontecchio MJ, et al. Diminishing the self-stigma of mental illness by coming out proud. Psychiatry Res. 2015;229:148–54.
Rüsch N, Abbruzzese E, Hagedorn E, Hartenhauer D, Kaufmann I, Curschellas J, et al. Efficacy of Coming Out Proud to reduce stigma’s impact among people with mental illness: pilot randomised controlled trial. Br. J. Psychiatry [Internet]. 2014 [cited 2018 Jun 28];204:391–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24434073 .
Corrigan PW, Rüsch N, Scior K. Adapting disclosure programs to reduce the stigma of mental illness. Psychiatr. Serv. [internet]. 2018 [cited 2018 Jun 28];appi.Ps.2017004. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29606076 .
Download references
Acknowledgments
We are grateful to the interviewees for their participation. We would like to thank Dr. Magdalena C. Meana, Dr. Ma. Luisa Babaran-Echavez, and barangay health workers for their assistance with data collection.
Availability of data and materials
The transcripts from the interviews are confidential and will not be shared.
Author information
Authors and affiliations.
Graduate School of Health Sciences, Kobe University, 701, 2-6-2, Yamamoto-dori, Chuo-ku, Kobe, Hyogo, 650-0003, Japan
Chika Tanaka & Hiroya Matsuo
City Health Office, City Government of Muntinlupa, Muntinlupa, Philippines
Maria Teresa Reyes Tuliao
Hyogo Institute for Traumatic Stress, Kobe, Japan
Eizaburo Tanaka
Kobe City College of Nursing, Kobe, Japan
Tadashi Yamashita
You can also search for this author in PubMed Google Scholar
Contributions
CT had a major role in the conception of the study, undertook the data collection, carried out the data analysis, and had a major role in writing the manuscript. MT contributed to the design of the study, assisted the data collection and interpretation, and supervised writing the manuscript. ET assisted data collection, conducted data analysis, and revised the manuscript. YT assisted data collection and revised the manuscript. HM supervised the design of the study, had a role in data analysis, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chika Tanaka .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the ethical committee of the Graduate School of Health Sciences, Kobe University, Japan (reference number 561). The study was conducted in accordance with the ethical guidelines set forth by the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects provided by the Ministry of Health, Labour, and Welfare of Japan. The City Health Office of the local government approved a head of time our study protocol, especially ethical aspects for potentially participating citizens. Potential participants received written and oral information about the study. It was emphasized that participation was voluntary. During the data collection, we obtained written consent from all the interviewees and verbal assent from PMHP whose carers participated in the interviews. In the case where the interviewee was under 18 years old, we gained verbal assent from them and written consent from their parents.
Consent for publication
Participants were informed that the information they shared in the interviews would be published in anonymised form. Written informed consent for publication was obtained.
Competing interests
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Interview guide for interviews with people with mental health problems. A set of questions we referred while interviewing PMHP. (DOCX 88 kb)
Additional file 2:
Interview guide for interviews with carers and community health volunteers. A set of questions we referred while interviewing carers and community health volunteers. (DOCX 90 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Tanaka, C., Tuliao, M.T.R., Tanaka, E. et al. A qualitative study on the stigma experienced by people with mental health problems and epilepsy in the Philippines. BMC Psychiatry 18 , 325 (2018). https://doi.org/10.1186/s12888-018-1902-9
Download citation
Received : 20 December 2017
Accepted : 20 September 2018
Published : 05 October 2018
DOI : https://doi.org/10.1186/s12888-018-1902-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Discrimination
- Mental illness
- The Philippines
- Qualitative
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]
Systematic Review of Cultural Aspects of Stigma and Mental Illness among Racial and Ethnic Minority Groups in the United States: Implications for Interventions
Affiliations.
- 1 San Francisco State University, San Francisco, CA, USA.
- 2 University of California San Francisco, San Francisco, CA, USA.
- 3 University of Texas Southwestern Medical Center, Dallas, TX, USA.
- 4 Teachers College, Columbia University, New York, NY, USA.
- 5 New York University Langone Health, New York, NY, USA.
- 6 New York University School of Global Public Health, New York, NY, USA.
- 7 Columbia Mailman School of Public Health, New York, NY, USA.
- PMID: 33811676
- DOI: 10.1002/ajcp.12516
Stigma is integral to understanding mental health disparities among racial and ethnic minority groups in the United States. We conducted a systematic review to identify empirical studies on cultural aspects of mental illness stigma (public, structural, affiliative, self) among three racial and ethnic minority groups (Asian Americans, Black Americans, Latinx Americans) from 1990 to 2019, yielding 97 articles. In comparison studies (N = 25), racial and ethnic minority groups often expressed greater public and/or self-stigma than White American groups. In within-group studies (N = 65; Asian American, n = 21; Black American, n = 18; Latinx American; n = 26), which were primarily qualitative (73%), four major cultural themes emerged: 1) service barriers including access and quality (structural stigma); 2) family experiences including concealment for family's sake, fear of being a burden, and stigma extending to family (affiliative stigma); 3) lack of knowledge about mental illness and specific cultural beliefs (public stigma); and 4) negative emotional responses and coping (self-stigma). These findings confirmed stigma has both similar and unique cultural aspects across groups. Despite this, few studies tested stigma reduction interventions (N = 7). These cultural insights can inform contextual change at the health systems and community levels to reduce stigma, and empowerment at the interpersonal and individual levels to resist stigma.
Keywords: Culture; Ethnicity; Mental illness; Race; Stigma; Systematic review.
© Society for Community Research and Action 2021.
Publication types
- Systematic Review
- Ethnic and Racial Minorities
- Mental Disorders*
- Minority Groups
- Racial Groups
- United States

COMMENTS
Mental health stigma is arguably the fundamental issue in the entire mental health field, including developmental psychopathology, given its impact on every participant in the enterprise ...
The Stigma and Discrimination Research toolkit is a collection of evidence and resources related to stigma and discrimination research. Health-related stigma and discrimination research has produced theories, models, frameworks, measures, methods, and interventions that can be applied across conditions and populations to help reduce the impact of stigma and discrimination.
In this paper, we integrate research specific to mental illness stigma with the more general body of research on stereotypes and prejudice to provide a brief overview of issues in the area. The impact of stigma is twofold, as outlined in Table 1. Public stigma is the reaction that the general population has to people with mental illness.
Anti-stigma activities in Singapore have been conducted by the state psychiatric institution, the Institute of Mental Health (IMH), the National Council of Social Service, the Health Promotion Board (statutory boards), and non-profit organisations such as the Singapore Association for Mental Health and Silver Ribbon Singapore, who have the ...
1. What is stigma? Stigmatizing attitudes contain some core assumptions. Media analyses of film and print have identified three common misconceptions about people with mental illness: they are homicidal maniacs who should be feared; they are rebellious, free spirits; or they have childlike perceptions of the world that should be marveled .Independent factor analyses from Canada, England and ...
Research into mental health stigma has largely focused on investigating this concept in adults , much less is known about young people with depressive symptoms and the stigma they experience [50, 67, 94]. More research is needed to better understand public and internalized stigma in these populations [32, 38].
The findings highlight that people with mental health conditions are aware of and experience stigma and discrimination across core domains of daily life. The importance of recognising the key role PWLEs can play in efforts to reduce stigma and discrimination was highlighted, and how they can be appropriately supported to contribute and have their experiential expertise recognised.
Background Stigma towards people with mental health problems (PMHP) is known to have substantial negative impacts on their lives. More in-depth exploration of the stigma and discrimination experienced by PMHP in low- and middle-income countries is needed. Previous research suggests that negative attitudes towards PMHP are widespread among the Filipino general public. However, no study has ...
Stigma is integral to understanding mental health disparities among racial and ethnic minority groups in the United States. We conducted a systematic review to identify empirical studies on cultural aspects of mental illness stigma (public, structural, affiliative, self) among three racial and ethnic minority groups (Asian Americans, Black Americans, Latinx Americans) from 1990 to 2019 ...
Research consistently shows that individuals with mental illness are subject to stigma and treated, or thought of, less favorably than others due to their mental health challenges (Gaebel et al., 2017).The detrimental impacts of stigma are far-reaching, impacting access to education, employment, housing, social support, and health care, adding to and amplifying the burden of mental illness ...