- Open access
- Published: 26 August 2024

Jordanian nursing students’ experience of harassment in clinical care settings
- Arwa Masadeh 1 ,
- Rula Al-Rimawi ORCID: orcid.org/0000-0002-7486-0957 2 ,
- Aziza Salem ORCID: orcid.org/0000-0001-9402-9282 3 &
- Rami Masa’deh ORCID: orcid.org/0000-0003-2762-7375 1
BMC Nursing volume 23 , Article number: 587 ( 2024 ) Cite this article
47 Accesses
Metrics details
Introduction
Nursing students experienced various types of bullying and abuse in their practice areas. This study aims to assess the incidence, nature, and types of bullying and harassment experienced by Jordanian nursing students in clinical areas.
Methodology
A cross-sectional, descriptive design was used, utilizing a self-report questionnaire. A convenient sampling technique was used to approach nursing students who are in their 3rd or 4th year in governmental and private universities.
Of 162 (70%) students who reported harassment, more than 80% of them were females and single. Almost 40% of them reported that males were the gender of the perpetrator. Almost 26.5% of them reported that patient’s relatives or friends were the sources of harassment. Psychological/verbal harassment was the most reported type of harassment (79%). Findings showed that there was a statistically significant difference in psychological/verbal harassment based on gender and type of the university. Also, there were significant negative correlations between psychological/verbal harassment, professional achievement, and personal life.
Harassment in the clinical area is affecting the professional and personal lives of students, who lack the knowledge of policy to report this harassment.
Key messages
1. Most of the students who reported harassment were females and single.
2. Psychological/verbal harassment was the most reported type of harassment.
3. Psychological/verbal harassment affected the students’ professional and personal achievements.
Peer Review reports
The healthcare sector is one of the most subjected sectors to violence among all sectors. Between 8 and 38% of healthcare providers exposed to workplace violence (WPV) in their career [ 1 ]. Nationally, the chief of the Jordan Medical Association declared that about 10 attacks on healthcare workers are recorded every month [ 2 ]. Among all healthcare workers, nurses and physicians are the most vulnerable personnel to WPV [ 3 , 4 ], as nurses have more contact with patients and their families or relatives.
Not only nurses are susceptible to WPV, but nursing students also are subjected to various types of violence, bullying, and harassment in their practice areas [ 5 , 6 , 7 , 8 , 9 ]. The prevalence of bullying among nursing students varies based on many factors. There were significant variations in the prevalence of bullying among nursing students, ranging from 9 to 96%, according to an integrative literature review that included 30 articles and examined the issue in addition to other factors [ 10 ]. In Australia, a study reported that half of 888 nursing students experienced bullying in the last year [ 6 ]. Similarly, an Omani study found that 53.4% of 118 nursing students experienced at least one incident of bullying during their practice period [ 5 ].
Nursing students experienced various types of bullying and abuse in their practice areas including verbal, emotional, physical, sexual, and racial abuse [ 5 , 8 , 11 , 12 , 13 , 14 ]. The most common form of abuse nursing students experienced was verbal abuse [ 6 , 8 , 12 ]. Students are mostly bullied by other nursing or medical students, nurses, physicians, other healthcare teams, school faculty, or their instructor [ 15 ], patients or their families [ 6 , 8 , 11 , 12 ], other hospital workers [ 6 ].
All forms of bullying and harassment have negative consequences on students, personally, physically, and emotionally; they might feel anxiety [ 12 , 16 , 17 , 18 ], sickness, low self-esteem [ 12 , 17 , 18 ], anger [ 12 , 17 , 19 ], fear, depression [ 12 , 15 , 19 ]. Additionally, bullying and harassment have an impact on students’ performance; they may cause them to be hesitant to visit clinical areas, doubt the quality of care they provide because it undermines their confidence, or reconsider their careers as nurses [ 5 , 6 , 12 , 15 , 19 ].
With all the negative consequences of bullying, most nursing students don’t report the incidents of bullying they have experienced [ 6 , 11 , 13 , 20 ]. Many students consider it to be part of the nursing profession [ 6 , 11 ], i.e. the “normalization” of bullying and violence [ 13 ]. Other students hated to be seen as victims [ 6 ], and others think that even if they reported the harassment, no action would be taken [ 6 , 20 ].
There is little known about nursing students’ experience, consequences, and reporting of bullying and harassment. Based on the literature review, there are many Jordanian studies on violence against nurses, but there is no published study investigating nursing students’ experience of bullying and harassment in Jordan, [ 21 ]. This study aims to assess the incidence, nature, and types of bullying and harassment experienced by Jordanian nursing students in clinical areas.
Materials and methods
Utilizing a self-report questionnaire, a cross-sectional, descriptive design was used, as very little is known about bullying and harassment of nursing students in Jordan.
The study was conducted at Nursing Faculties in five governmental and five private universities. Governmental universities are located in the north, middle, and south of Jordan. Four of them have the largest number of nursing students among all governmental and private universities. Three private universities are located in the Capital and two are in the north of Jordan. There are very few private universities outside the Capital. Approached private universities have the largest number of nursing students among all private universities.
Non probability, convenient sampling technique was used. We approached nursing students who met the inclusion criteria: who were in their 3rd or 4th year of study and willing to participate. The sample size was determined based on Cohen power primer [ 22 ]. Using a conventional power of 0.8, medium effect size of 0.25, level of significance of 0.05, and Pearson Correlation, the minimum sample size would be 134. Using G-power 3.1.9.2, and using the power of 0.8, medium effect size (0.25), and level of significance of 0.05 and Pearson r, the minimum total sample size would be 138 [ 23 ].
The questionnaire in the current study was adapted from Hewett [ 24 ]. The questionnaire consists of six parts, including (a) demographic (including Age, Gender, Marital Status, and Wearing Hijab for females) and educational data (including Year of Study, Type of Program, and University type), (b) verbal (12 items), physical (8 items), and sexual harassment (6 items) in clinical areas, (c) data about the perpetrator (12 items) and the settings (3 items) where the harassment occurred, (d) impact of harassment on personal life (8 items) and professional achievement (5 items), (e) reporting of harassment in clinical areas (one question about if the student reported the harassment or not and 6 items about the reason behind not-reporting the incident), and (f) management of violence in clinical areas (one open-ended question). The tool consists of 67 items; each item rated the occurrence of harassment or the impact of harassment on a four-point Likert scale (0 ―Never to 3 – Often: more than 5 times). Items about reporting the harassment were yes or no questions. The internal consistency of the questionnaire revealed Cronbach’s alpha of 0.88. Originally, the tool was developed in English. It was translated in compliance with WHO translation guidelines [ 25 ]. Community health and mental health nursing professionals evaluated the questionnaire after it had been translated and before the pilot study was carried out to ensure the study instruments’ content validity. The research process - from distributing questionnaires to receiving data - was tested, and no problems were found.
Data collection
After obtaining approval from the Institutional Review Board (IRB) of Applied Science Private University’ committees, the principal investigator approached the deans of Nursing Faculties and explained the study’s purpose and procedure. Then, a poster about the study with a barcode of the online questionnaire was displayed in the hall of all nursing faculties. The participant read the cover letter before filling out the questionnaire, which explained the purpose of the study, the role of the participants, their right to withdraw from the study, and all their information would be anonymous and confidential.
Ethical considerations
Ethical approvals from the Applied Science Private University as well as from all other participating universities were obtained before commencing the research. Besides, this research was conducted under the principles of the Declaration of Helsinki.
Data Analysis
Data were analyzed using SPSS (version 25). The study sample and their responses were described using descriptive statistics. Differences in participants’ scores based on their characteristics were assessed by running a series of t-tests. Further, Pearson coefficient was used to detect relationships between the participants’ characteristics and harassment scores.
In this study, 268 nursing students were approached, 244 consented and 230 of them fully completed and returned the questionnaires; those were involved in the final analysis. All nursing students involved in this study have attended at least one clinical placement course and were either in their third or fourth year of study. Data was divided into two groups (i.e. group one: students who reported facing harassment; and group two: students who did not report any type of harassment).
Description of the participants
Table 1 shows the characteristics of nursing students based on the occurrence of harassment. Concerning the total participated nursing students (the two groups), approximately, 70% ( N = 162) of them reported that they faced harassment. Female students formed almost 80% of the overall sample. Most of the students were single with a mean age of 22.37 ± 3.156. Participated students were enrolled in the university either in the regular program or bridging program with almost half of the students from governmental universities and half of them from private universities.
Regarding the group of students who reported harassment (i.e. group one), more than 80% ( N = 182) of them were females and single. Almost 40% ( N = 65) of them reported that males were the gender of the perpetrator. Nursing students were asked about the source of harassment and almost 20% ( N = 33) of them showed that doctors were the sources of harassment, 17.9% ( N = 29) reported that patients were the source of harassment, 37.7% ( N = 61) were patients relatives or friends and 19.8% ( N = 32) administrative staff were the source of harassment. Almost two-thirds 66% ( N = 107) of those who stated they were harassed didn’t know about the policy of reporting harassment. Psychological/verbal harassment was the most reported type of harassment, representing approximately 79% ( N = 142) of those reported harassment.
The difference in harassment based on the characteristics of the participants
Several independent sample t-tests were conducted to examine the difference in psychological/verbal harassment; physical harassment, and sexual harassment based on the gender of the student, marital status, type of the university, type of the program, and previous work experience. These statistical tests were only conducted for students who reported the occurrence of harassment (group one). Findings showed that there were no statistical differences in physical and sexual harassment based on all previous variables.
About psychological/verbal harassment, Table 2 shows that there was a statistically significant difference in psychological/verbal harassment based on gender and type of the university. Female students reported significantly higher levels of psychological/verbal harassment (M = 22.14, SD = 7.29) than male students (M = 19.31, SD = 4.74); t (60.976) = -2.61, p-value 0.011. Eta squared was 0.04 indicating that the magnitude of the difference was small. Moreover, students from private universities reported significantly higher levels of psychological/verbal harassment (M = 22.60, SD = 7.06) than those from governmental universities (M = 20.42, SD = 6.73); t (155.086) = -2.008, p-value 0.046. Eta squared was 0.024 indicating that the magnitude of the difference was small. There were no statistical differences in psychological/verbal harassment based on marital status, type of the program, and previous work experience.
The correlation between psychological/verbal harassment, professional achievement, personal life, and age of nursing students
Pearson r product-moment correlation coefficient was used to examine the relationship between psychological/verbal harassment, professional achievement, personal life, and age of nursing students. Table 3 shows that there were statistically significant moderate negative correlations between psychological/verbal harassment, professional achievement, and personal life ( r =-0.437, p-value < 0.001; r =-0.566, p-value < 0.001, respectively). An increase in psychological/verbal harassment was significantly associated with a decrease in the professional achievement and personal life of the students. The R-squared between psychological/verbal harassment, and professional achievement is 0.19 indicating that almost 19% of the change in the variance of professional achievement is explained by psychological/verbal harassment. Again, the R-squared between psychological/verbal harassment and personal life is 0.32 indicating that almost 32% of the change in the variance of personal life is explained by psychological/verbal harassment. However, findings showed that there was no significant correlation between age and psychological/verbal harassment.
Nursing students spend around 20 h weekly in the clinical area after the first year. They are on the first line of encounter not only with patients and their relatives, but also with nurses, physicians, and other health team members. The study reveals that 70% ( n = 162) of students in the sample were subjected to one or more types of harassment, which is considered a little bit lower than what was reported by Abd El Rahman and Mabrouk [ 17 ] who conducted their research in Egypt found that (88%) of the sample faced bullying during their clinical rotation. On the other hand, this result is higher than the Omani study which found that 53.4% of students experienced harassment at least once throughout their clinical rotation [ 5 ]. Also, it was higher than what was reported by Birks and colleagues; who compared Australian and British students and found that (50.1%) and (35.5%) respectively, were bullied among students in their sample [ 26 ]. Additionally, it was higher than a New Zealand study which revealed that 40% of students experienced harassment in clinical areas [ 16 ]. A higher percentage of bullying among nursing students could be attributed to underestimating student’s knowledge, skills, and experiences.
The study revealed that most of the bullied students (80%) were females. This is not strange as the majority of the sample were female too. These results are comparable with an Omani study [ 27 ]. However, a study found that Australian females were subjected to harassment more than male students, while this was not the case for British students [ 26 ]. Over the world, the nursing profession is considered a female profession; this could be the case because females are more compassionate and capable to care of people in health and sickness.
The study revealed that 40% of the reported gender of perpetrators were males. This was inconsistent with what was found by Palaz, who found that the majority of perpetrators were females (92.4%) [ 28 ]. Whereas, the perpetrators in the current study were 26.5% patient’s relatives or friends, 20% doctors, 18% patients, and 13.9% administrative staff. Omani study found that patients (42.3%) and their relatives (33.9%) were the major perpetrators, followed by other healthcare teams (31.4%), doctors (28%), and registered nurses (26%) [ 5 ]. Whereas, the key perpetrators of verbal abuse in Hong Kong were patients (66.8%), followed by hospital staff (29.7%), university supervisors (13.4%), and patients’ relatives (13.2%) [ 29 ]. The students have to contact with different individuals with varying educational backgrounds, cultural backgrounds, ethical perspectives, and value systems. However, many students have low self-esteem and limited communication skills, especially in clinical settings, as they are considered new and stressful areas [ 5 ].
Despite the large number of harassed nursing students, two-thirds of them don’t know about reporting harassment policy (66%). This was very close to a study conducted in Oman that found victims of harassment were unaware of any regulations against harassment in in college (60.2%) or clinical areas (65.2%) [ 11 ]. On the other hand, 36% of students in the current study reported that they didn’t report any incident as nothing would be done. Budden and colleagues reported that many participants knew about such policies, whether in the university (65.5%) or clinical settings (69%). Despite students’ knowledge of policies, these were not clear, they feared being mistreated, thought that nothing would be done if reported, didn’t know how and where to report, thought that the incidence was not significant to report [ 6 ], and the most frightening idea is that harassment is considered a normal part of the job [ 6 , 11 , 26 ].
The current study revealed that most students 79% reported subjecting to psychological/verbal harassment. This result supports the previous studies conducted worldwide; such as 60% in Turkey [ 28 ], 73.3% in Iran [ 30 ], and 55% in Saudi Arabia [ 31 ]. Although a smaller percentage was reported for verbal harassment in Hong Kong (30.6%), it was higher than that for physical abuse (16.5%) [ 29 ]. Nursing students weren’t subject to physical harassment, they were subjected to psychological/verbal harassment or sexual harassment as gestures without reaching the point of physical harassment. Also, the perpetrator is subjected more to legal liability for this type of harassment.
Sexual harassment was reported only in 2.5% of nursing students in the current study, this result was less than what was reported by Tollstern and colleagues, who found that 9.6% of respondents training at a local hospital in Tanzania reported subjecting to sexual harassment [ 32 ]. Also, the results of a Chinese meta-analysis revealed that the incidence of sexual harassment among female nursing students was 7.2% [ 33 ]. On the other hand, a shocking high result of sexual harassment was reported in Korea, where it was found that 50.8% of the participants faced sexual harassment. The sexual harassment was reported as gender-linked harassment; as 98% of perpetrators were male [ 34 ]. Closing one’s way, touching one’s body on purpose, and attempting to have sex, all these fluctuating behaviors in reported sexual harassment might be related to cultural, religious, and behavioral differences between countries [ 32 ]. Furthermore, an integrative review revealed that sexual harassment among nursing students is exacerbated by near body contact care role of nursing, the perceptions of societies toward nursing as a women’s profession, the sexualization of nurses, and the imbalances in the workplace [ 35 ]. In our society, we are governed by customs and traditions emanating from our Islamic religion. Therefore, compared to other studies, the frequency of sexual harassment in the current study is considered very low.
Although our finding revealed no statistical differences in sexual harassment based on all variables in the study including gender, this could be connected to the low incidence of sexual harassment in the current study. However, the systematic review and other studies worldwide revealed that female nurses are facing a high prevalence of sexual harassment [ 35 , 36 , 37 ].
On the contrary to what was reported by Budden and colleagues and Cheung and colleagues, our results revealed a statistically significant difference in psychological/verbal harassment based on the gender and type of the university [ 6 , 29 ]. This could be related to the fact that the sample consisted primarily of female students. Students at private universities reported much higher levels of verbal and psychological harassment than those at governmental universities. These governmental universities are located in areas considered conservative compared to those where private universities are located.
The current study found significant moderate negative correlations between psychological/verbal harassment, professional achievement, and personal life. Professional achievement and personal life tend to decrease as verbal harassment increases. These results are not surprising and are supported by what was found in a Chinese study, which reported a significant increase in sick leave taken after verbal abuse that lasted to ten days. Furthermore, the researchers revealed the presence of a significant negative effect of verbal harassment on personal feelings, clinical performances, and the extent to which they were disturbed by verbal harassment [ 29 ]. In the same context, Amoo and colleagues revealed that bullying caused a loss of confidence and the occurrence of stress and anxiety among nursing students [ 7 ].
Implications
The current study showed that most of the students who were subjected to harassment didn’t know that there was a policy that addressed this problem. Nursing faculty, health organizational administration, and nursing instructors are responsible for implementing strategies that will end the sequence of all types of harassment and promote a healthy work environment through; improving students’ communication skills, empowering them, establishing and planning goal-directed training programs related to harassment and harassment prevention in clinical area for nursing students before starting their training. Also, it is very important to teach students that harassment should never be tolerated, no matter how it manifests or where it comes from.
The nursing curriculum must be updated to add new topics such as communication skills, and how to deal with perpetrators of different types of harassment. Moreover, the clinical area must have clear policies regarding reporting harassment which should be declared to students. Furthermore, studies are needed regarding the psychological effects of harassment, and how to deal with the psychological effects, to help student manage their fears and negative feelings related to harassment. The literature indicated that many nurses quit or change careers as a result of harassment, so it’s critical to focus on adapting to a zero-harassment environment [ 38 , 39 ].
Strengths and limitations
Strengths of this study include recruiting samples from all geographical areas in Jordan; north, middle, and south, and from governmental and private universities. Despite the strengths of this study, its results should be considering its limitations. There were not enough male students in the sample; further study may adequately recruit male students. Another limitation is not including nationality in the questionnaire, so generalization to all Arabic or other students might be limited. Therefore, it is recommended to replicate this study among various Arabic populations.
This study indicates that harassment is a significant issue among Jordanian nursing students. Nursing students face different types of harassment all over the journey of clinical training. Results showed a high prevalence of psychological/ verbal abuse that affected the professional and personal lives of students. Despite the high incidence of harassment among nursing students, most students have not reported the harassment officially as they lack the knowledge of how to report this harassment or are not aware of the presence of policies regarding harassment, highlighting the importance of providing education to increase their awareness about such policies. The study highlights the role of universities in developing training programs and policies, if none, to prevent harassment in clinical areas and manage the effect of harassment among students. This will contribute in creating a safe, healthy, and supportive educational environment for nursing students.
Data availability
Data cannot be shared openly but are available on request from authors.
WHO. Preventing violence against health workers: World Health Organization. 2022. https://www.who.int/activities/preventing-violence-against-health-workers .
Why Physicians. and Nurses are Attacked? Jordan News. 2022.
Bernardes MLG, Karino ME, Martins JT, Okubo CVC, Galdino MJQ, Moreira AAO. Workplace violence among nursing professionals. Revista Brasileira De Med do Trabalho. 2020;18(3):250.
Article Google Scholar
Liu J, Gan Y, Jiang H, Li L, Dwyer R, Lu K, et al. Prevalence of workplace violence against healthcare workers: a systematic review and meta-analysis. Occup Environ Med. 2019;76(12):927–37.
Article PubMed Google Scholar
Qutishat MG, Kannekanti S. Bullying and harassment perceived by undergraduate nursing students in clinical settings, and its implication to academic strategies and interventions. J Health Sci Nurs. 2019;4(9):56–62.
Google Scholar
Budden LM, Birks M, Cant R, Bagley T, Park T. Australian nursing students’ experience of bullying and/or harassment during clinical placement. Collegian. 2017;24(2):125–33.
Amoo SA, Menlah A, Garti I, Appiah EO. Bullying in the clinical setting: lived experiences of nursing students in the Central Region of Ghana. PLoS ONE. 2021;16(9):e0257620.
Article PubMed PubMed Central CAS Google Scholar
Samadzadeh S, Aghamohammadi M. Violence against nursing students in the workplace: an Iranian experience. Int J Nurs Educ Scholarsh. 2018;15(1).
Jafarian-Amiri SR, Zabihi A, Qalehsari MQ. The challenges of supporting nursing students in clinical education. J Educ Health Promotion. 2020;9:216.
Fernández-Gutiérrez L, Mosteiro‐Díaz MP. Bullying in nursing students: a integrative literature review. Int J Ment Health Nurs. 2021;30(4):821–33.
Qutishat MG. Underreporting bullying and harassment perceived by undergraduate nursing students: a descriptive correlation study. Int J Mental Health Psychiatry. 2019;5(1).
Özcan NK, Bilgin H, Tülek Z, BOYACIOĞLU NE. Nursing Students’ Experiences of Violence: A Questionnaire Survey. J Psychiatric Nursing/Psikiyatri Hemsireleri Dernegi. 2014;5(1).
Hallett N, Wagstaff C, Barlow T. Nursing students’ experiences of violence and aggression: a mixed-methods study. Nurse Educ Today. 2021;105:105024.
Ehsani M, Farzi S, Farzi F, Babaei S, Heidari Z, Mohammadi F. Nursing students and faculty perception of academic incivility: a descriptive qualitative study. J Educ Health Promotion. 2023;12(1):44.
Baraz S, Memarian R, Vanaki Z. Learning challenges of nursing students in clinical environments: a qualitative study in Iran. J Educ Health Promotion. 2015;4(1):52.
Minton C, Birks M, Cant R, Budden LM. New Zealand nursing students’ experience of bullying/harassment while on clinical placement: a cross-sectional survey. Collegian. 2018;25(6):583–9.
Abd El Rahman RM. Perception of student nurses’ bullying behaviors and coping strategies used in clinical settings. 2014.
Birks M, Budden LM, Biedermann N, Park T, Chapman Y. A ‘rite of passage?’: bullying experiences of nursing students in Australia. Collegian. 2018;25(1):45–50.
Hashim N, Aziz HAM, Amran MAA, Azmi ZN. Bullying among nursing students in UiTM Puncak Alam during Clinical Placement. Environment-Behaviour Proc J. 2020;5(15):49–55.
Albakoor FA, El-Gueneidy MM, El-Fouly OM. Relationship between coping strategies, bullying behaviors and nursing students’ self esteem. Alexandria Sci Nurs J. 2020;22(1):47–58.
Jordanian Database for Nursing Research Jordan: School of Nursing, The University of Jordan. 2017. http://jdnr.ju.edu.jo/home.aspx .
Cohen J. A power primer. Psychol Bull. 1992;112(1):155.
Article PubMed CAS Google Scholar
Faul F. G*Power. 3.1.9.2 ed. Germany2014. p. Statistical Power Analysis Program.
Hewett D. Workplace violence targeting student nurses in the clinical areas: Stellenbosch. University of Stellenbosch; 2010.
WHO. Process of translation and adaptation of instruments. Geneva: World Health Organization; 2018.
Birks M, Cant RP, Budden LM, Russell-Westhead M, Özçetin YSÜ, Tee S. Uncovering degrees of workplace bullying: a comparison of baccalaureate nursing students’ experiences during clinical placement in Australia and the UK. Nurse Educ Pract. 2017;25:14–21.
Qutishat MEGM. Bullying and harassment perceived by undergraduate nursing students in clinical settings and its implication to academic strategies and interventions. J Health Sci Nurs. 2019;9(4).
Palaz S. Turkish nursing students’ perceptions and experiences of bullying behavior in nursing education. J Nurs Educ Pract. 2013;3(1):23.
Cheung K, Ching SS, Cheng SHN, Ho SSM. Prevalence and impact of clinical violence towards nursing students in Hong Kong: a cross-sectional study. BMJ open. 2019;9(5):e027385.
Article PubMed PubMed Central Google Scholar
Samadzadeh S, Aghamohammadi M. Violence against nursing students in the workplace: an Iranian experience. Int J Nurs Educ Scholarsh. 2018;15(1):20160058.
Shdaifat EA, AlAmer MM, Jamama AA. Verbal abuse and psychological disorders among nursing student interns in KSA. J Taibah Univ Med Sci. 2020;15(1):66–74.
PubMed PubMed Central Google Scholar
Tollstern Landin T, Melin T, Mark Kimaka V, Hallberg D, Kidayi P, Machange R, et al. Sexual harassment in clinical Practice—A cross-sectional study among nurses and nursing students in Sub-saharan Africa. SAGE Open Nurs. 2020;6:2377960820963764.
Zeng LN, Zong QQ, Zhang JW, Lu L, An FR, Ng CH, et al. Prevalence of sexual harassment of nurses and nursing students in China: a meta-analysis of observational studies. Int J Biol Sci. 2019;15(4):749–56.
Kim TI, Kwon YJ, Kim MJ. Experience and perception of sexual harassment during the clinical practice and self-esteem among nursing students. Korean J Women Health Nurs. 2017;23(1):21–32.
Smith E, Gullick J, Perez D, Einboden R. A peek behind the curtain: an integrative review of sexual harassment of nursing students on clinical placement. J Clin Nurs. 2023;32(5–6):666–87.
Kahsay WG, Negarandeh R, Dehghan Nayeri N, Hasanpour M. Sexual harassment against female nurses: a systematic review. BMC Nurs. 2020;19(1):58.
Maghraby RA, Elgibaly O, El-Gazzar AF. Workplace sexual harassment among nurses of a university hospital in Egypt. Sex Reproductive Healthcare: Official J Swed Association Midwives. 2020;25:100519.
Yeh T-F, Chang Y-C, Feng W-H, sclerosis, Yang M. C-C. Effect of Workplace Violence on Turnover Intention: The Mediating Roles of Job Control, Psychological Demands, and Social Support. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2020;57:0046958020969313.
Hollowell A. Violence affects nursing recruitment, retention, NNU report finds. USA: National Nurses United; 2024.
Download references
Acknowledgements
The authors thank Applied Science Private University for supporting this study. Also, the authors thank the participants and the deans of the nursing faculties.
Not Applicable.
Author information
Authors and affiliations.
School of Nursing, Applied Science Private University, Amman, 11937, Jordan
Arwa Masadeh & Rami Masa’deh
Nursing College, Al-Balqa Applied University, Salt, Jordan
Rula Al-Rimawi
Nursing Department, University of Tabuk, Tabuk, Saudi Arabia
Aziza Salem
You can also search for this author in PubMed Google Scholar
Contributions
Concepts: A.M. & R.M Design: A.M. & R.M Definition of intellectual content: A.M. & R.M Literature search: A.M. & R.R. Data acquisition: A.M. & R.M Data analysis: A.M. & R.M Statistical analysis: R.M. Manuscript preparation: A.M. & A.S Manuscript editing: A.M. & A.S Manuscript review: A.M. & A.S & R.F.
Corresponding author
Correspondence to Rami Masa’deh .
Ethics declarations
Ethics approval and consent to participate.
IRB approval was obtained from the IRB committee in Applied Science Private University (2021-2022-5-1). The principal investigator posted a poster about the study with a barcode of the online questionnaire in the hall of all nursing faculties. The participant read the cover letter before filling out the questionnaire, which explained the purpose of the study, the role of the participants, their right to withdraw from the study, and all their information would be anonymous and confidential. Filling out the questionnaire was considered as a consent form. So, informed consent was obtained implicitly from all subjects.
Consent for publication
Not Applicable (as explained before).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Masadeh, A., Al-Rimawi, R., Salem, A. et al. Jordanian nursing students’ experience of harassment in clinical care settings. BMC Nurs 23 , 587 (2024). https://doi.org/10.1186/s12912-024-02146-x
Download citation
Received : 24 May 2024
Accepted : 02 July 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s12912-024-02146-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological harassment
- Physical harassment
- Sexual harassment
- Personal Life
- Professional Achievement
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 31 March 2023
Education program promoting report of elder abuse by nursing students: a pilot study
- Dahye Park 1 &
- Jeongmin Ha 2
BMC Geriatrics volume 23 , Article number: 204 ( 2023 ) Cite this article
1851 Accesses
1 Citations
1 Altmetric
Metrics details
Elder abuse is an important public health concern that requires urgent attention. One main barrier to active responses to elder abuse in clinical settings is a low level of relevant knowledge among nurses. This study aims to develop an educational program to promote an intent to report elder abuse among nursing students and assess its effectiveness, with a focus on the rights of older adults.
A mixed method design was used with the Analyze, Design, Develop, Implement, and Evaluate model. Twenty-five nursing students from Chungbuk Province participated in the study. Attitude toward older adults and knowledge of, awareness of, attitude towards, and intent to report elder abuse were assessed quantitatively and analyzed using paired t-test. The feasibility of the program and feedback were collected qualitatively through group interviews and analyzed using content analysis.
After the education program, attitude toward older adults (Cohen’s d = 1.08), knowledge of (Cohen’s d = 2.15), awareness of (Cohen’s d = 1.56), attitude towards (Cohen’s d = 1.85), and intent to report elder abuse (Cohen’s d = 2.78) increased, confirming the positive effects of this program. Overall, all participants were satisfied with the contents and method of the program.
Conclusions
The method of program delivery should be improved and tailored strategies to boost program engagement among nursing students should be explored to implement and disseminate the program.
Peer Review reports
Introduction
Elder abuse is an important public health concern with serious social, economic, and health consequences [ 1 ]. In Korea, a 2011 survey of 10,674 older adults aged 65 years and above showed that 12.6%—about one out of every eight older adults—suffered abuse [ 2 ]. Moreover, although recent surveys on elder abuse are unavailable, considering the rise in the incidence of elder abuse during the coronavirus disease 2019 (COVID-19) pandemic in the United States [ 3 ], the incidence of elder abuse in Korea may have also increased.
In clinical practice, nurses are likely to witness or predict elder abuse as their work involves a careful observation of patients’ daily lives, which provides them with an opportunity to detect, treat, and prevent elder abuse [ 4 ]. However, nurses do not actively intervene or connect older adults suffering from abuse to relevant intervention programs, despite having opportunities [ 5 ]. This is because of severe barriers to active reporting of elder abuse (e.g., invisibility and caregiver risk factors are common) [ 6 ]. Indeed, the number of reports of elder abuse by mandated reporters in 2021 was only 860 out of 7,634—a decline of 8.4% from the 939 reported cases of elder abuse by mandated reporters in 2020 [ 7 ].
In most autonomous districts in Korea, visiting nurses provide care to older adults belonging to vulnerable groups in the community [ 8 ]. Visiting nurses can determine whether the environment is safe to prevent elder abuse, which is easily concealed in the community, and have the opportunity to detect elder abuse early [ 9 ]. However, Korean nurses’ awareness of elder abuse was lower than that of other occupational groups such as nursing care workers and paramedics [ 9 ]. As Korean nurses’ awareness of elder abuse was low, there is a great possibility that on witnessing elder abuse while on duty they may not recognize it or cope with it effectively [ 9 ].
Nurses’ understanding of elder abuse is an important factor for active responses to elder abuse in a clinical setting. However, nursing students in Korea display poor knowledge on elder abuse [ 10 ]. A previous study that investigated Korean nursing students’ elder abuse-related educational needs exploring the difference between the levels of importance and performance using the IPA analysis found that the highest priority knowledge set that must be urgently improved included topics of adults’ physical and emotional changes, sexual abuse, legal punishment for elder abuse, roles of mandated reporters, roles of older adult protection agencies and shelters for elder abuse victims, encouragement of reporting and hotline, and process following abuse reporting [ 4 ]. Furthermore, topics comprising the second priority group of knowledge set that must be gradually improved consisted of human rights for older adults, roles of mandated reporters for protecting older adults’ rights, roles for prevention, verbal abuse, physical abuse, emotional abuse, neglect, and abandonment [ 4 ].
Data showing that professional knowledge about elder abuse is a potent antecedent to reporting elder abuse [ 5 ] highlights the need for a systematic educational program for nursing students in Korea, including expert knowledge about elder abuse, reporting of abuse, and legal and ethical grounds. However, studies that have developed and implemented elder abuse-related educational programs for nursing students in Korea are limited. This study aims to develop an educational program for promoting the intent to report elder abuse among nursing students and assess its effectiveness using the Reach, Efficacy of program under optimal conditions (i.e., intervention study), Adoption, Implementation, Maintenance) framework, an approach frequently mentioned in implementation and dissemination research [ 11 , 12 , 13 ]. We sought to assess the first two out of five elements of the framework: (1) to promote intent to report elder abuse incidents and to investigate the effects of the education program on attitude toward older adults, knowledge of, awareness of, attitude towards, and intent to report elder abuse; (2) to collect feedback from users through group interviews and analyze the feedback using content analysis to improve the feasibility of the program.
Study design
This pilot study aims to develop an education program for promoting intent to report elder abuse incidents among nursing students and to examine the feasibility of the program nationwide. After developing the program, we used a mixed method design to collect baseline data to pivot the program for effective adoption in practice (Fig. 1 ). We used one group pretest–posttest design in this pilot study to develop and assess the educational program, aiming to improve intent to report elder abuse among nursing students.
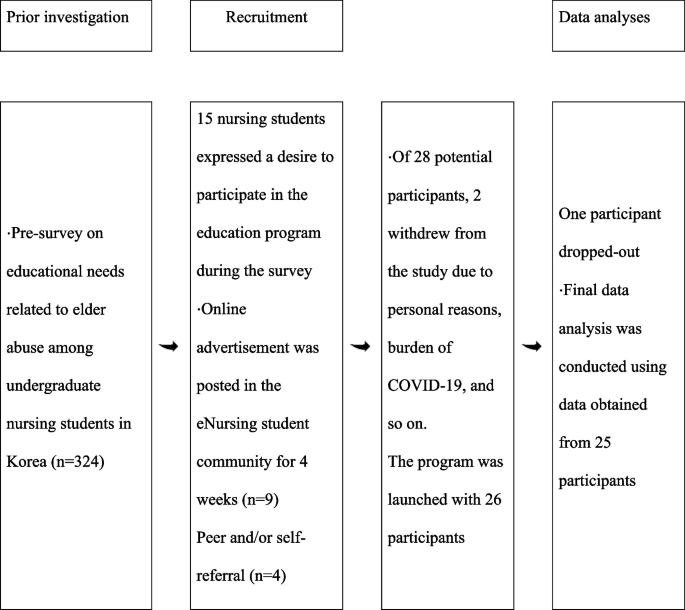
The process of participant recruitment
Study participants
Nursing students were set as the study population and the only eligibility criterion was the ability to participate in four sessions of education provided on an offline platform over two months. There were no other criteria, including age and gender. There are no established standards for sample determination for pilot studies. Thus, we determined our sample size with reference to the previous findings that suggested the optimal sample size to be 10–30 participants with the same characteristics as the targeted study population [ 11 , 14 ]. In consideration of four sessions of education over a period of two months, we recruited 28 nursing students for this pilot study.
Figure 1 shows the participant recruitment process. First, in the preliminary study on the educational needs for elder abuse among nursing students, we advertised the elder abuse-related education program and asked students who were interested to leave their phone numbers. Of 324 survey respondents, 15 showed interest in the program and left their phone numbers.
Next, we posted an advertisement on an online bulletin board for nursing students for four weeks from September 3, 2020, to October 3, 2020, and nine nursing students showed interest in participating in the study. Four students were additionally recruited through peer and self-referral. However, 2 of 28 nursing students who showed interest in the study withdrew their decision to participate in the study during the informed consent process either for personal reasons or due to COVID-19 restrictions.
Ethical consideration
This study was approved by the Institutional Review Board at S University (IRB No S**-2020–08-011). The participants were informed about the purpose of the study, voluntary participation, freedom to withdraw from the study, guarantee of anonymity, and use of collected data for only research purposes, and written consent was obtained after confirming that the participants have accurately understood the purpose, procedure, and method of the study using the talk-back method.
Study procedure
Development of education program.
The education program used as the intervention in this study was developed based on the Analyze, Design, Develop, Implement, and Evaluate model, a widely used generic model for instructional design [ 15 ]. This model comprises five steps: analysis, designing, development, implementation, evaluation as shown in Table 1 .
Implementation of the education program
A 240-min offline education program developed by the researchers for nursing students was provided over four Saturday sessions. The details of the program are shown in Table 2 . This program’s design differed from existing programs as it not only comprised frontal teaching, but also more participative methods, such as brain writing. Brain writing, a teaching and learning method known to effectively collect ideas and solve problems, was applied. The contents included in this program were: understanding of older adults’ rights and abuse, definition and types of elder abuse, current status and laws pertinent to elder abuse, professional older adult protective agencies, and tips for reporting elder abuse.
Instruments
Before beginning offline education, we administered a survey to examine participants’ attitudes toward older adults, knowledge of, awareness of, attitude towards, and intent to report elder abuse. The same survey was administered immediately after the program was completed. Furthermore, group interviews were conducted using semi-structured questions after education to obtain feedback about the program and improve its feasibility.
Attitude toward older adults
Attitude toward older adults was measured using the Semantic Differential Scaling developed by Sanders et al. [ 16 ] and adapted by Im [ 17 ]. This instrument comprises 20 pairs of contradictory adjectives, and each adjective pair is rated on a seven-point Likert scale (1 = very negative, 7 = very positive). In a previous study, seven items (#1, 2, 3, 6, 7, 10, 15, 18) were reverse coded to maintain consistency in scoring. The average score of 20 items was used; a higher score indicated a positive attitude toward older adults, with a score of 3.5–4.5 indicating a neutral attitude [ 16 ]. The reliability (Cronbach's α) of the scale was 0.90 at the time of development, 0.82 in the study by Im [ 17 ], 0.80 at the baseline, and 0.82 at the post-test in this study.
Knowledge about elder abuse reporting
Knowledge about elder abuse reporting was measured using a 12-item questionnaire. The first author developed this questionnaire based on previous studies and the Welfare of the Senior Citizens Act, which includes the regulations for punishment for elder abuse (Article 55–2, 3, 4; Article 57), duty and procedure of elder abuse reporting (Article 39–6), and older adult protective agencies (Article 39–5). The questionnaire comprised two items for definition (concept and type), five items for law (mandated reporter and organizations), and five items for system (reporting organization and process). Participants were asked to check “I don’t know” or “I am well aware of it,” which were scored as 0 and 1, respectively. The total possible score for knowledge about elder abuse reporting ranged from 0–12, and a higher score indicated a greater level of knowledge. The Cronbach’s α was 0.77 at the baseline and 0.82 at the post-test in this study.
Awareness of elder abuse
Awareness of elder abuse offences was measured using 12 scenarios developed by Moon and Williams [ 18 ] and translated and adapted in Korea by Yoo and Kim [ 19 ]. The 12 scenarios are divided into five domains: physical abuse, emotional abuse, financial abuse, sexual abuse, and neglect. Specifically, there were three physical abuse scenarios (scenarios 1, 3, 4), four emotional abuse scenarios (scenarios 2, 5, 6, 10), two financial abuse scenarios (scenarios 8, 11), two neglect scenarios (scenarios 7, 9), and one sexual abuse scenario (scenario 12). Each scenario was rated on a five-point Likert scale from 1 “This is not an abuse” to 5 “This is a very serious abuse.” The mean overall score and scores by domain were used. The total score ranged from 12–60, and a higher score indicated greater awareness of elder abuse. The reliability (Cronbach’s α) score was 0.77 in the study by Yoo and Kim [ 19 ], 0.66 at the baseline, and 0.72 at the post-test in this study.
Attitude toward elder abuse
Attitude toward elder abuse was measured using the tool developed for older adults by Cho [ 20 ]. This 25-item tool comprises fourteen items for attitude, four items for subjective norms, and seven items for perceived behavioral control. Each item is rated on a four-point Likert scale (1 “strongly disagree,” 2 “disagree,” 3 “agree,” 4 “strongly agree”), with a higher score indicating more positive attitude toward intervening in the situation. Some examples of the items for attitude include “If I report an elder abuse incident, the organization that receives the report will take necessary actions,” and “Intervening in elder abuse will be helpful for the older adult involved.” There were four items for subjective norms, but two items pertinent to coworkers and head nurse were deleted because our participants were students. The scores rated on a four-point scale were summed. Cronbach’s α of the scale was 0.77 for attitude, 0.74 for subjective norms, and 0.73 for perceived behavioral control in a previous study, and 0.72 for the baseline and 0.84 for the post-test in this study.
Intent to report
Intent to report was assessed by having the participants answer yes (1) or no (0) to the question asking whether they will report each of the 12 hypothetical scenarios presented earlier. The total score was calculated by summing the score for 12 scenarios [ 18 ]. Cronbach’s α was 0.64 at the baseline and 0.68 at the post-test in this study.
Group interview to obtain feedback for elder abuse education program
At the end of the program, a group interview was conducted using semi-structured questions to collect feedback on the 4-week program. The three semi-structured questions used were: “What motivated you to participate in the program?”; “What were some of the positive experiences and difficulties you faced while participating in the program?”; “What should the researchers consider when revising the education program for nursing students?”.
Data collection and analysis
The data were collected between September 3, 2020, and April 31, 2021. Of the 28 nursing students who showed interest to participate in the study, 26 were enrolled in the study, and 25 out of the 26 completed the program. Quantitative data collected from one student who withdrew in the middle of the program was excluded from the analysis, so data from 25 participants were included in the final quantitative analysis. Quantitative analysis was performed using SPSS 25.0 software, and the reliability of the instruments, frequency, and descriptive statistics were analyzed. The differences in the scores before and after education were compared using paired t-test. The effect size was calculated using Cohen’s d due to the small sample size. The normality of the data was tested using the Shapiro–Wilk test, and normal distributions of attitude toward older adults, knowledge of, awareness of, attitude towards, and intent to report elder abuse were checked.
The interview was conducted by the first author, who had experience in qualitative research. The researcher used a list of semi-structured questions and audio-recorded the interviews. Further, an assistant researcher observed participants’ reactions and took field notes as necessary. The interviews were transcribed, and the first author and another author independently performed content analysis to extract themes by category, theme clusters, and categorization.
Participants’ sociodemographic characteristics
Table 3 shows the participants’ sociodemographic characteristics. The majority of participants were women (88.0%), and the mean age was 21.8 years, ranging from 20–28 years. Only 10 participants had prior education about elder abuse or exposure to an elder abuse awareness campaign before enrolling in the study. Regarding intervening in an elder abuse case, 12 participants stated that they would only report the incident before the education, while 4 stated that they would do so after the program. Moreover, before the education, 2 participants indicated that they would report the incident and intervene with only the older adult, while after the program, 10 stated that they would do the same.
Effects of the education program on intent to report elder abuse among nursing students
After the program, nursing students’ attitude toward older adults (Cohen’s d = 1.08), knowledge (Cohen’s d = 2.15), awareness (Cohen’s d = 1.56), attitude (Cohen’s d = 1.85), and intent to report elder abuse (Cohen’s d = 2.78) increased, confirming the positive effects of the program.
Table 4 shows the results before and after the education.
Attitude toward older adults significantly increased from 80.88 ± 11.39 at the baseline to 92.4 ± 9.84 after education (t = -6.38, p = 0.028, Cohen’s d = 1.08). Knowledge about elder abuse significantly increased from 4.76 ± 1.79 at the baseline to 8.84 ± 1.99 after education (t = -12.13, p < 0.001, Cohen’s d = 2.15). Awareness of elder abuse significantly increased from 45.16 ± 5.38 at the baseline to 52.32 ± 3.57 after education (t = -8.75, p < 0.001, Cohen’s d = 1.56). By domain, the scores for physical abuse (t = -5.25, p < 0.001), emotional abuse (t = -7.21, p < 0.001), financial abuse (t = -2.37, p = 0.026), and neglect (t = -4.13, p < 0.001) statistically significantly increased.
Attitude toward elder abuse significantly increased from 56.16 ± 3.90 at the baseline to 63.12 ± 3.61 after education (t = -7.41, p < 0.001, Cohen’s d = 1.85). By domain, the scores for attitude (t = -5.23, p < 0.001), subjective norms (t = -4.55, p < 0.001), and perceived behavioral control (t = -3.27, p = 0.003) statistically significantly increased.
Intent to report elder abuse significantly increased from 32.08 ± 1.73 at the baseline to 39.76 ± 3.50 after education (t = -9.21, p < 0.001, Cohen’s d = 1.08).
Participants’ feedback on education program for promoting nursing students’ intent to report elder abuse
Reason for participating in the program.
The reasons for participating in the program included self-improvement ( n = 2), increased perceived need for education after the informed consent process ( n = 1), exploring topics for course assignment ( n = 1), perceived need for education during practicum ( n = 5), perceived need for education while providing care for families of older adults ( n = 1), and had an interest in the topic ( n = 1). The participants were satisfied with the education program overall.
Benefits and challenges of the program
Learning about care for older adults.
Students mentioned learning about different types of elder abuse and laws pertaining to elder abuse as a benefit of participating in the program. Furthermore, they also stated that they can utilize what they have learned to provide more meaningful care for older adults.
Developing competencies as a nursing student (formal Para).
Most students stated that they liked the fact that the education program was free and that they participated to learn instead of just passing an exam. Unlike other education programs, they were allowed to relieve their skepticism about nursing by interacting with their fellow students proudly about nursing and engaging in introspection, based on which they were able to better recognize the value of nursing.
Feedback for improving the feasibility of the program
Need to emphasize that the program is about reporting elder abuse.
Many nursing students who saw the advertisement poster misunderstood the program as a geriatric nursing program when they were recruited. Thus, the students advised that we emphasize the program as an educational program for nursing students whose prospective mandates reporting elder abuse.
Development of an e-learning program
With in-person activities restricted during the COVID-19 pandemic, students suggested developing strategies that allow more nursing students to access the program. For example, they recommended converting the offline program to an e-learning program for promoting intent to report elder abuse.
This pilot study aimed to develop an educational program to promote intent to report elder abuse among nursing students and assess its effectiveness. Additionally, we aimed to collect feedback from participants to improve the feasibility of the program. After administering the developed education program about elder abuse, students showed improved attitudes toward older adults, knowledge of, awareness of, attitude towards, and intent to report elder abuse, confirming the positive effects of the program.
These results support the findings of a previous study that investigated awareness, subjective norms, perceived behavioral control, and attitude toward elder abuse among nursing students in Korea, where students who took a relevant course demonstrated a higher level of awareness, subjective norms, and perceived behavioral control [ 10 ]. Therefore, continuously providing a systematic education program on elder abuse reporting to nursing students, especially during a time witnessing various instances of elder abuse due to the burgeoning older adult population [ 21 ] and Korean nurses’ awareness of elder abuse being low compared to other occupational groups in Korea [ 9 ], will not only bolster nursing students’ competencies for responding to elder abuse incidents but will also contribute to addressing the crucial societal issue. However, it is necessary to update how the program is promoted and modify the current program, particularly in light of comments that various platforms of operation should be explored to facilitate the implementation and dissemination of the program. Therefore, we will discuss three factors that should be improved.
First, the title of the program should be chosen such that the contents of the program are clearly conveyed when advertising the program. The objective of the education program developed in this study was to educate nursing students about their duty to report elder abuse. However, some participants misunderstood the program as an educational program for geriatric nursing during the recruitment process. Further, none of the participants in the program demonstrated an interest in elder abuse reporting or an increased desire to improve their ability to report the same. Therefore, the title of the program should reflect nursing students’ opinions. Students’ opinions can be collected by asking them to choose from a list of a few titles. Further, considering that a contest enhances the credibility of a company and boosts individuals’ willingness to be involved in the said company [ 22 ], launching a naming contest for the program could attract students’ attention, deepen their understanding of the program, and increase the participation rate.
Second, the instructors need to use questions that trigger thinking to give students adequate opportunities to think about the topic (reporting elder abuse) on their own and discuss it among them. The students reported that they experienced a positive emotional process where they felt more value in nursing as they contemplated about a topic with fellow students and engaged in introspection and reflection. Nurses in geriatric hospitals in Korea experience ethical conflicts as “being distressed,” namely moral distress, which refers to being unable to do the right thing despite being aware of it [ 23 ]. One main cause of nurses’ distress is a working environment that does not fulfill ethical obligations [ 23 ]. In East Asian contexts, elder abuse is pervasively perceived as a personal family issue. Family matters and issues are kept within the family, as sharing them with outsiders can expose the family to public embarrassment and lead to loss of face. Besides, other reasons why older adults remain silent include a culture‐specific misunderstanding of elder abuse, shame, self‐blame, and the belief of inescapable ill fate [ 24 ].
Therefore, mandated reporters in Korea choose not to execute mandatory reporting because they feel that by modifying the conditions that cause abuse, family members can participate in providing care for older adults at home. They believe that providing care at home, improving the relationship between older adults and their families, and intermediation provides a better cultural option for older adults [ 25 ]. Additionally, older Korean adults, as victims, expressed reluctance to seek help or attention despite abuse experiences due to a culture of family honor and filial piety, an obligation to uphold norms, such as endurance and self-effacement, and belief in fatalism (acceptance of fate) [ 24 ]. To address this problem, education programs using verified teaching methods, such as the nudge strategy, and exemplary cases that arouse moral emotions advancing from the conventional moral education focused on character and virtue towards a cognitive approach should be actively developed [ 26 ].
Third, a non-face-to-face education program should be developed. We could not expect students’ active participation amid restrictions on in-person activities due to the COVID-19 pandemic. The students also suggested that a non-face-to-face education program should be developed. In a recent study, nurses and social workers who participated in virtual-reality-based elder abuse and neglect educational intervention acquired knowledge about identifying elder abuse and neglect and demonstrated 99% accuracy in their decisions for mandatory reporting. Further, the knowledge and skills they acquired in the intervention brought positive changes in their actual work performance [ 27 ]. These results suggest that a non-face-to-face education program can adequately alter knowledge and teaching skills that may have a positive impact in a clinical setting. Therefore, developing a non-face-to-face version of our program would provide effective education for a larger population of nursing students.
This pilot study aims to develop an educational program to promote the intent to report elder abuse among nursing students and assess its effectiveness. Despite the strength—developing and examining the effectiveness of an education program about elder abuse reporting based on nursing students’ educational needs—this study has a few limitations. First, some participants misunderstood this program as an education program for geriatric nursing instead of elder abuse. This misunderstanding could have contributed to the lower scores found on the pre-test. Thus, the educational goal should be clarified and promoted in the process of participant recruitment to confirm this program’s effectiveness in the follow-up study. Second, all participants were students at a single school. Additionally, students volunteered to participate in this offline program while all other courses were administered online, which indicates that only students with high educational needs may have been recruited. Thus, our findings cannot be generalized. Studies including nursing students from various regions and diverse demographic backgrounds are needed. In summary, future research should focus on planning preventive measures for elder abuse, developing suitable training programs, and supporting the older adult population. The method of program delivery should be improved and tailored strategies to boost program engagement among nursing students should be explored to implement and disseminate the program.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Yon Y, Ramiro-Gonzalez M, Mikton CR, Huber M, Sethi D. The prevalence of elder abuse in institutional settings: A systematic review and meta-analysis. Eur J Public Health. 2019;29(1):58–67. https://doi.org/10.1093/eurpub/cky093 .
Article PubMed Google Scholar
Lee YJ, Kim Y, Park JI. Prevalence and factors associated with elder abuse in community-dwelling elderly in Korea: Mediation effects of social support. Psychiatry Investig. 2021;18(11):1044. https://doi.org/10.30773/pi.2021.0156 .
Article PubMed PubMed Central Google Scholar
Han SD, Mosqueda L. Elder abuse in the COVID-19 era. J Am Geriatr Soc. 2020;68(7):1386–7. https://doi.org/10.1111/jgs.16496 .
Ha J, Park D. Educational needs related to elder abuse among undergraduate nursing students in Korea: an importance-performance analysis. Nurse Educ Today. 2021;104:104975. https://doi.org/10.1016/j.nedt.2021.104975 .
MohdMydin FH, Othman S. Elder abuse and neglect intervention in the clinical setting: perceptions and barriers faced by primary care physicians in Malaysia. J Interpers Violence. 2020;35(23–24):6041–66. https://doi.org/10.1177/0886260517726411 .
Article Google Scholar
Miller CA. Nursing for wellness in older adults. Lippincott Williams & Wilkins; 2009; 162.
Ministry of Health and Welfare. Elder Abuse in Korea. 2019. https://www.korea.kr/archive/expDocView.do?docId=40008
Ministry of Health and Welfare. Guideline of integrated health promotion in communities. 2021. http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=0320&CONT_SEQ=364090 . Accessed 20 Mar 2023.
Park JH, Cho CM. Community nurses’ perceptions of elder abuse based on an ecological system model: a descriptive study. J Korean Gerontol Nurs. 2022;24(4):412–23. https://doi.org/10.17079/jkgn.2022.24.4.412 .
Lee YJ, Kim YS. A study on the influence of nursing students’ perception, subjective norms and perceived behavior control on attitudes toward elder abuse. J Korea Acad-Industr Cooperat Soc. 2018;19(5):410–7. https://doi.org/10.5762/KAIS.2018.19.5.410 .
Estabrook B, Zapka J, Lemon SC. Evaluating the implementation of a hospital work-site obesity prevention intervention: applying the RE-AIM framework. Health Promot Pract. 2012;13(2):190–7. https://doi.org/10.1177/1524839910385897 .
Wozniak L, Rees S, Soprovich A, Al Sayah F, Johnson ST, Majumdar SR, Johnson JA. Applying the RE-AIM framework to the Alberta’s caring for diabetes project: a protocol for a comprehensive evaluation of primary care quality improvement interventions. BMJ Open. 2012;2(5):e002099. https://doi.org/10.1136/bmjopen-2012-002099 .
Brownson RC, Colditz GA, Procto EK. Dissemination and implementation research in health: Translating science to practice. 2nd ed. England: Oxford University Press in England, Inc; 2012.
Hil R. What sample size is “enough” in internet survey research? Interpersonal Computing and Technology. An Electronic Journal for the 21st Century. 1998;6(3–4):1–12.
Dick W, Carey L, Carey JO. The systematic design of instruction, 7th ed. United States: Allyn & Bacon in the United States. 2011.
Sanders GF, Montgomery JE, Pittman JF, Balkwell C. Youth’s attitudes toward the elderly. J Appl Gerontol. 1984;3(1):59–70. https://doi.org/10.1177/073346488400300107 .
Im YS. Knowledge and attitude toward the elderly of a general hospital nurses [Unpublished Master’s thesis, Chosun University]. 2002.
Google Scholar
Moon A, Williams O. Perceptions of elder abuse and help-seeking patterns among African-American, Caucasian American, and Korean-American elderly women. Gerontol. 1993;33(3):386–95. https://doi.org/10.1093/geront/33.3.386 .
Article CAS Google Scholar
Yoo SH, Kim CS. A study of old persons' subjective perceptions on elder abuse. In: Korean Institute of Gerontology: a study of the current state and a countermeasure on elder abuse. Korea: Korean Institute of Gerontology in Korea; 2004. p. 9–39.
Cho YK. Influencing factors on nurses’ intention of intervening in elder abuse [Master Thesis, Yonsei university]. 2014.
Kong J, Jeon H. Functional decline and emotional elder abuse: a population-based study of older Korean adults. J Fam Violence. 2018;33:17–26.
Kim YH. The study of the contest exhibition on corporate image and behavior intention. J Korea Content Assoc. 2017;17(12):590–9.
Kim M, Oh Y, Kong B. Ethical conflicts experienced by nurses in geriatric hospitals in South Korea: “if you can’t stand the heat, get out of the kitchen.” Int J Environ Res Public Health. 2020;17:4442.
Lee Y-S, Moon A, Gomez C. Elder mistreatment, culture, and help-seeking: a cross-cultural comparison of older Chinese and Korean immigrants. J Elder Abuse Negl. 2014;26:244–69.
Doe SS, Han HK, McCaslin R. Cultural and ethical issues in Korea’s recent elder abuse reporting system. J Elder Abuse Negl. 2009;21:170–85.
Engelen B, Thomas A, Archer A, Van de Ven N. Exemplars and nudges: Combining two strategies for moral education. J Moral Educ. 2018;47(3):346–65. https://doi.org/10.1080/03057240.2017.1396966 .
Pickering CE, Ridenour K, Salaysay Z, Reyes-Gastelum D, Pierce SJ. EATI Island–a virtual-reality-based elder abuse and neglect educational intervention. Gerontol Geriatr Educ. 2018;39(4):445–63. https://doi.org/10.1080/02701960.2016.1203310 .
Download references
Acknowledgements
The authors wish to sincerely thank the participants of this study.
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2020S1A5A8046754). The funding source had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and affiliations.
Department of Nursing, Semyung University, 65 Semyung-Ro, Jechoen-Si, Chungbuk, Republic of Korea
Department of Nursing, Dong-A University, 3 Dongdaeshin-Dong Seogu, Busan, 602–714, Republic of Korea
Jeongmin Ha
You can also search for this author in PubMed Google Scholar
Contributions
Ha contributed to the conception and design of the study, and discussion. Park contributed to the conception and design of the study, theoretical introduction and discussion, acquisition of data, analysis and interpretation of data. Ha and Park were a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jeongmin Ha .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board at Semyung University (IRB No SMU-2020–08-011). The participants were informed about the purpose of the study, voluntary participation, freedom to withdraw from the study, guarantee of anonymity, and use of collected data for only research purposes, and written informed consent was obtained after confirming that the participants have accurately understood the purpose, procedure, and method of the study using the talk-back method. All methods were carried out in accordance with relevant guidelines and regulations (e.g., Helsinki declaration).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Park, D., Ha, J. Education program promoting report of elder abuse by nursing students: a pilot study. BMC Geriatr 23 , 204 (2023). https://doi.org/10.1186/s12877-023-03931-0
Download citation
Received : 15 December 2022
Accepted : 25 March 2023
Published : 31 March 2023
DOI : https://doi.org/10.1186/s12877-023-03931-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- ADDIE model
- Elder abuse
- Education program
- Nursing students
BMC Geriatrics
ISSN: 1471-2318
- General enquiries: [email protected]
Protecting Our Seniors From Abuse & Neglect

Recent Elder Abuse in Nursing Homes: Case Studies
Elder abuse is far more common than many people would like to believe. What’s worse, recent reports confirm that nursing home abuse skyrocketed during the COVID-19 pandemic. Help keep your loved ones safe by reading these recent case studies on elder abuse in nursing homes. Accepting that elder abuse is a real problem is the first step in preventing it.
Examples of Elder Abuse in Nursing Homes: A Nationwide Problem
Nursing home abuse happens when trust is violated through an act — or a failure to act — that harms an older person. It can include emotional, financial, physical, or sexual abuse as well as nursing home neglect.
Tragically, a 2020 report from the World Health Organization (WHO) estimates that roughly 1 in 6 adults 60 years old and over were the victims of elder abuse in nursing homes and other community settings.
Even worse, the WHO warns that this already alarming figure is likely to be too low since only 1 in 24 cases of elder abuse is ever reported.
Recent case studies on elder abuse in nursing homes show that this is, unfortunately, a nationwide problem.
The most common forms of nursing home abuse are:
- Emotional abuse : when an older person is yelled at, threatened, or belittled
- Nursing home neglect : substandard care of a nursing home resident
- Physical abuse : any form of violence that leaves an older person significantly injured, including cases of wrongful death
- Sexual abuse : any sexual contact with an elder who cannot give their consent
Thankfully, help is available if you or a loved one suffered nursing home abuse or neglect. Get a free case review to see if you can access legal compensation right now.

Get a free legal case review if you or a loved one has suffered abuse or neglect.
Examples of Case Studies on Elder & Nursing Home Abuse
1. suspected nursing home abuse in massachusetts.
After hundreds of 911 calls were made about suspected nursing home abuse, a criminal investigation is underway against an assisted living facility in Watertown, Massachusetts.
Several of the heartbreaking reports include:
- After responding to a call about a faulty ventilator, firefighters found that none of the electrical outlets in a resident’s room were working
- An injured nursing home resident was on the floor asking for help, but when firefighters asked the staff member in charge about it, she just laughed
- Firefighters found staff performing CPR on a man who had already been dead for hours
Further, in a case of suspected physical abuse at the same nursing home, the daughter of a dementia patient found her mother’s face severely battered.
“It was horrific. She had a huge gash on her forehead and a lump the size of a golf ball, her whole face was bruised.” – Daughter of Massachusetts nursing home resident
These examples reveal a widespread pattern of abuse and neglect by staff, which will hopefully be corrected. No nursing home resident should ever have to endure these hardships.
2. Nursing Home Sexual Abuse in Minneapolis
A male caregiver at a Minneapolis care facility was sentenced to eight years in prison for the rape of a nursing home resident with Alzheimer’s disease.
“My final memories of my mother’s life now include watching her bang uncontrollably on her private parts for days after the rape, with tears rolling down her eyes, apparently trying to tell me what had been done to her, but unable to speak.” – Daughter of sexual abuse victim
A follow-up investigation by CNN revealed that the rapist had assaulted multiple other residents, including those who suffered from mental or physical handicaps, before he was finally caught.
3. Nursing Home Neglect in Iowa
A nursing home resident in Iowa died after extreme neglect related to dehydration . The emergency room doctor believes she died from a stroke after not receiving any type of fluid for at least four to five days. The nursing home was fined $77,463.
Examples of Elder Abuse in Nursing Homes During the Pandemic
While nursing home abuse and neglect were already a very serious issue, the ongoing coronavirus pandemic made things even worse.
According to Human Rights Watch, neglect and isolation may be responsible for causing severe damage to countless nursing homes residents during the COVID-19 crisis.
Recent nursing home abuse case studies revealed:
- A resident in her 80s who was healthy and pre-pandemic died shortly after visitation stopped due to suspected malnutrition
- In less than a year, a dementia patient living in a nursing home went from 106 pounds to 82 pounds before being discharged and dying several days later
- A dementia patient in her 70s lost 20 pounds during the pandemic and developed painful bedsores on her buttocks and toes
Why Does Elder Abuse Happen in Nursing Homes?
Elder abuse in nursing homes is believed to occur for several reasons.
Nursing home abuse may happen due to:
- Understaffing
- Inadequate staff training, especially in dementia care
- Lack of supervision
- Staff burnout
No matter what the explanations for elder abuse are, it is never acceptable. All nursing home residents deserve to be free from harm and properly cared for.
How Common Is Elder Abuse?
Although there is a lack of concrete data, recent reports suggest that elder abuse is common.
It is believed that elder abuse is more likely to occur with nursing home residents than with older adults living in community settings. In fact, 2 in 3 nursing home staff members admitted to abusing or neglecting residents in the 2020 WHO report.
Common Signs of Nursing Home Abuse
The most common signs of nursing home abuse are physical symptoms and any type of sudden change in behavior.
Depending on the form, some additional signs of nursing home abuse may include:
- Bruising, scars, or welts seen on the body
- Mumbling, sucking one’s thumb, or rocking
- Unexplained STDs or other genital infections
- Bedsores, malnutrition, or dehydration
Get Help For Elder Abuse in Nursing Homes
If you or a loved one was the victim of nursing home abuse, you may be entitled to compensation. Money awarded in a nursing home lawsuit can help pay for medical expenses and bring peace of mind.
The Nursing Home Abuse Center is dedicated to helping victims of nursing home neglect, abuse, and wrongful death. Contact us now to find out if we can help you and your family.

The Nursing Home Abuse Center (NHAC) was founded to bring justice to those affected by nursing home and elder abuse. Our mission is to educate and empower victims of abuse and their families to take a stand against this unlawful mistreatment. We work to return dignity back to those who have been broken down by nursing home abuse and neglect.
- BMC Health Services Research. (2020). Elder Abuse And Neglect: An Overlooked Patient Safety Issue. A Focus Group Study Of Nursing Home Leaders’ Perceptions Of Elder Abuse And Neglect. Retrieved August 14, 2021 from https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-5047-4
- Fiandaca, C. (2021). I-Team: Watertown Long-Term Care Facility Investigated For Possible Abuse, Neglect. CBS Boston. Retrieved from August 14, 2021 https://boston.cbslocal.com/2021/02/12/long-term-care-facility-nursing-home-elder-abuse-investigation/
- Human Rights Watch. (2021). Us: Concerns Of Neglect In Nursing Homes. Retrieved August 14, 2021 from https://www.hrw.org/news/2021/03/25/us-concerns-neglect-nursing-homes
- Merrilees, A. (2019). '83 Years Old, Unable To Speak, Unable To Fight Back.' Daughters Share Heartbreaking Stories Of Abuse In Nursing Homes. ABC News. Retrieved from August 14, 2021 https://abcnews.go.com/Politics/83-years-unable-speak-unable-fight-back-daughters/story?id=61504444
- World Health Organization. (2021). Elder Abuse. Retrieved August 14, 2021 from https://www.who.int/news-room/fact-sheets/detail/elder-abuse
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Recognizing Elder Abuse: An Interprofessional Simulation Experience With Prelicensure Health Care Students
Cunningham, Shala PT, DPT, PhD 1 ; Cunningham, Cynthia RN, MSN, CHSE 2 ; Foote, Lisa BSN, MSN, CHSE 2
1 Department of Physical Therapy, Radford University, Roanoke, Virginia.
2 Clinical Simulation Centers, Radford University, Radford, Virginia.
Address correspondence to: Shala Cunningham, PT, DPT, PhD, Department of Physical Therapy, Radford University, 101 Elm Ave SE, Roanoke, VA 24013 ( [email protected] ).
The authors declare no conflicts of interest.
Background and Purpose:
A common role within all health care professions includes the ability to recognize and report elder abuse. However, teaching the characteristics and assessment of abuse can be difficult. To allow students to engage in a realistic case-based scenario within a health care team, an immersive simulation was developed involving the care of an elderly woman with signs of abuse. The purpose of this quasiexperimental study was to explore the influence of the experience on the participants' perceptions of interprofessional care and their understanding of the assessment of abuse.
Methods:
This study utilized a mixed-methods research design. A sample of convenience of nursing and physical therapy students (n = 143) from 3 institutions in southwest Virginia was utilized for this study. Participants' perceptions were assessed using the Interprofessional Socialization and Valuing Scale (ISVS) and through focus group interviews.
Results:
Students demonstrated a statistically significant improvement based on the Wilcoxon matched pairs test ( P < .001) on all 21 questions of the ISVS. A phenomenological study design was employed for qualitative analysis of focus group interviews performed postsimulation to generate information about the students' perceptions of the experience. Two themes emerged from the interviews: (1) communication as a team to provide wholistic patient care and (2) recognition of abuse.
Discussion:
The students reported an improved understanding of collaboration on a health care team and how to investigate potential abuse occurring in the home. This further supports research suggesting the importance of interactive learning techniques in teaching health care students to recognize symptoms of elder abuse.
Full Text Access for Subscribers:
Individual subscribers.

Institutional Users
Not a subscriber.
You can read the full text of this article if you:
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Physical therapists\' knowledge of physical elder abuse—signs, symptoms, laws, and facility protocols</strong>', 'saliga sue pt mhs ncs; adamowicz, connie bs, spt; logue, andrew mpt; smith, karen mpt', 'journal of geriatric physical therapy', 'april 2004', '27', '1' , 'p 5-12');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link"> physical therapists' knowledge of physical elder abuse—signs, symptoms, laws,..., physical therapist management of patients with suspected or confirmed..., essential components of physical therapist management of patients with..., apta geriatrics' guiding principles for best practices in geriatric physical....
- Advanced search

Advanced Search
Elder abuse: an approach to identification, assessment and intervention
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- For correspondence: [email protected]
- Figures & Tables
- Related Content
Elder abuse is increasingly recognized as an important problem associated with significantly increased rates of hospital admission, 1 nursing home placement 2 and mortality. 3 Estimates of prevalence vary widely, but recent studies, including a 2008 systematic review, have suggested that 5%–10% of older adults report experiencing abuse. 4 , 5
In December 2012, the Canadian Parliament passed Bill C-36, the Protecting Canada’s Seniors Act, which aims to protect older adults through amendments to the Criminal Code . This bill makes elder abuse an aggravating factor for sentencing purposes, such that criminal acts of elder abuse might be subject to maximal sentencing. There is, however, a substantial discrepancy between prevalence estimates of elder abuse and the number of cases reported to police. In 2009, for example, Canadian police reported 7871 cases of violent crime against people 65 years of age or older 6 (relative to a total population of over 4 million in that age group 7 ). Justice Canada researchers have found that charges were laid in only 17% of cases of alleged elder abuse handled by Ottawa police between 2005 and 2010. 8 These data suggest that many cases of elder abuse do not reach the criminal justice system and that physicians may be among the first who can intervene.
As populations age, it is becoming increasingly necessary for physicians to identify, assess and initiate management of elder abuse. Research into how best to do this is therefore of substantial importance.
The complexity of the issue, however, means that research into elder abuse is inherently challenging. For example, elder abuse is defined in various ways. The term encompasses multiple types of abuse, including physical, psychological, sexual and financial abuse, as well as neglect, each of which may be associated with different risk factors, mechanisms of causality and optimal interventional approaches. 9 – 11 Moreover, many older adults who experience abuse are cognitively impaired, socially isolated and frail, and they may have complicated and dependent relationships with their abusers. 12 – 14 Furthermore, the collection of sensitive information about abuse could have negative emotional, social, financial or legal consequences for multiple parties, leading both the abused older person and the abuser to actively try to hide the abuse. This raises ethical concerns about conducting research on a vulnerable population. 13 , 15 , 16
Given the challenges of conducting research in this topic area, there is little evidence to provide guidance on whether screening for abuse is effective and which interventions to manage the risk of abuse are effective. A previous systematic review of interventions for elder abuse showed the paucity of evidence. 17 The current review ( Box 1 ) updates that earlier systematic review; discusses definitions, risk factors, clinical manifestations and recommendations for screening for elder abuse; and offers an approach for clinicians to consider when assessing older adults at risk for abuse.
Evidence for this review
We searched MEDLINE, Embase, CINAHL and PsycINFO from the earliest date available to August 30, 2013, using a variety of search terms, including “elderly,” “abuse” and “mistreatment” (the full list of terms and the search strategy are available from the authors upon request). We included both primary research articles and relevant review articles, and we reviewed the reference lists of pertinent articles. We performed a systematic review of interventions for the management of elder abuse, the focus of our article, according to the same search strategy. A full description of our search and its findings, as well as details about the studies we found, is presented in Appendix 1 (available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.141329/-/DC1 ).
- How is elder abuse defined?
The concept of elder abuse is not consistently defined across jurisdictions in Canada. The World Health Organization adopted the United Kingdom Action on Elder Abuse definition in 1995 and defines it as “a single or repeated act or lack of appropriate action, occurring within any relationship where there is an expectation of trust which causes harm or distress to an older person.” 18
More specifically, abuse includes acts of both commission and omission, and encompasses physical abuse (acts with the intention of causing physical pain or injury, including hitting, kicking, slapping and pushing or the misuse of medications or restraints), psychological abuse (acts with the intention of causing emotional pain or injury, including humiliation, isolation and threats of harm or abandonment), sexual abuse (including any sexual act to which the older person has not consented, could not consent or was pressured into consenting), financial exploitation (the misappropriation of an older person’s money or property, including theft, fraud and pressuring the person to make changes to wills or financial transactions) and neglect (the failure of a caregiver to meet the needs of a dependent older person, including withholding of medications, nutrition or adequate shelter). 12 , 13 , 19
- What are the risk factors for elder abuse?
A recent systematic review (of medium methodologic quality) identified 13 risk factors for abuse among community-dwelling older adults ( Box 2 ). 14 The authors concluded that lack of consistency in definitions and measurement tools in this field limits the potency of the evidence and that further research is required.
Risk factors * for elder abuse identified in a recent systematic review 14
Relating to the older person:
Cognitive impairment
Behavioural problems
Psychiatric illness or psychological problems
Functional dependence (requiring assistance with activities of daily living)
Poor physical health or frailty
Low income or wealth
Trauma or past abuse
Ethnicity (increased risk among nonwhites for overall abuse, African Americans for financial abuse and Canadian Aboriginals for physical and sexual abuse)
Relating to the perpetrator:
Caregiver burden or stress
Relating to the relationship:
Family disharmony with poor or conflictual relationships
Relating to the environment:
Low social support
Living with others (except in financial abuse)
↵ * There is inconsistent evidence supporting some of these risk factors. See details in text.
However, the systematic review 14 focused on positive findings of factors associated with abuse and did not address conflicting studies with negative results showing that the same factors were not associated with abuse. Physical impairment and functional dependency, for example, were included as significant risk factors in the systematic review overall, but multiple studies included in the review also showed conflicting results that were not addressed. One of these studies was a prospective study of 341 Canadian patients served by a health and social service agency, which found that needing help with activities of daily living was not a significant predictor of abuse. 20 A cross-sectional survey of 412 older adults in Nanjing, China, also showed that physical impairment was not a significant risk factor. 21
A possible association between elder abuse and ethnicity is also inconsistent. For example, older nonwhite participants were more likely to be abused than white participants in a nine-year observational cohort study of 2812 community-dwelling older adults in Connecticut. 22 That study involved linking the cohort with protective service records for elderly people, which might have introduced reporting bias that could have resulted in overestimation of the effect of ethnicity. A more recent population survey of 5777 older adults in the United States showed that race- and ethnicity-based differences in the risk of elder abuse were absent after controlling for income, health status and social support. 23
There is also some evidence that living alone is a risk factor for abuse, including a cross-sectional survey of 2039 older adults in rural China, who represented 91% of the entire population over age 60 in 17 villages. 24 Another cross-sectional study, which involved 460 older adults in Spain, found that living with another person was a risk factor for abuse only if the other person had a mental illness or problems with alcohol or drug use. 25
These seemingly conflicting results may reflect different study designs, populations and definitions of abuse, but they may also be due to differences in risk factors for each type of abuse. For example, a cross-sectional survey of 676 older adults in Spain found that psychological abuse was associated with depressive symptoms, social isolation and bladder incontinence in the abused individual; neglect was associated with social isolation, use of social services and living alone; and financial abuse was associated with being single, age 85 years or older, and lower score on the Mini-Mental State Examination. 26 Beach and colleagues 27 found that African American older adults were at greater risk of financial and psychological abuse than non–African Americans in a cross-sectional study of 903 community-dwelling older adults in Pennsylvania. In another cross-sectional study, which involved 3005 community-dwelling older adults across the US, Latino older adults were at lower risk of verbal and financial mistreatment than whites. 28
These studies, which are summarized in Appendix 1 (available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.141329/-/DC1 ; see Part 3), suggest that, rather than attempting to study elder abuse as a whole, researchers may need to address each type of abuse individually. Most of the studies, however, were limited to self-reported abuse and did not use validated assessment tools for determining the presence of abuse.
- What are the clinical manifestations of elder abuse?
The clinical manifestations of elder abuse are difficult to identify and vary by type of abuse. Dyer and colleagues 29 conducted a nonsystematic literature review of forensic markers of elder abuse, defined as “factors that are relevant to medical and legal determinations of whether elder abuse or neglect has occurred.” They identified a variety of clinical features, including inadequately explained or unusual locations for skin abrasions, lacerations, bruises and burns; spiral fractures of long bones and fractures at sites other than the wrist, hip or vertebrae in a nonalcoholic elderly person; malnutrition and dehydration; pressure ulcers; sexually transmitted infections or pain in the oral or anal–genital region; and vaginal or rectal bleeding without other reasonable explanation.
Some other reviews on elder abuse have included lists of possible clinical manifestations, both including and in addition to those discussed by Dyer and colleagues. 29 However, we were unable to identify any primary studies reporting the prevalence or test characteristics of any symptoms or signs of elder abuse. There is thus poor evidence to support any of these markers.
- Are there recommendations for screening or case-finding for elder abuse?
In its 2013 systematic review for recommendations on elder abuse screening, the US Preventive Services Task Force 30 included only the Elder Abuse Suspicion Index. This two-minute, six-item questionnaire featuring dichotomous variables ( Box 3 ) was administered in private by family physicians to cognitively intact older adults in a primary care setting in Montréal. 31 When compared with a blinded social work assessment for identifying abuse, one or more positive responses on the Elder Abuse Suspicion Index had a sensitivity of 47% and a specificity of 75%. There was also an enthusiastic response to the index from family physicians in a post-study survey, which suggests its acceptability. Given the lack of studies on screening instruments, however, the US Preventive Services Task Force concluded that there was insufficient evidence to assess the balance between benefits and harms of screening all elderly adults for abuse and neglect, and the task force was therefore unable to make a recommendation about screening for the general elderly population. 30 The risk–benefit profile for screening in higher-risk populations is likely more in favour of screening, although there is no supporting evidence for this assumption.
Elder Abuse Suspicion Index 31
Questions 1–5 are asked of the patient and may be answered “Yes,” “No” or “Did not answer.” Question 6 is answered by the physician and may be answered “Yes,” “No” or “Not sure.”
Within the past 12 months:
Have you relied on people for any of the following: bathing, dressing, shopping, banking or meals?
Has anyone prevented you from getting food, clothes, medication, glasses, hearing aids or medical care or from being with people you wanted to be with?
Have you been upset because someone talked to you in a way that made you feel shamed or threatened?
Has anyone tried to force you to sign papers or to use your money against your will?
Has anyone made you afraid, touched you in ways that you did not want or hurt you physically?
Doctor: Elder abuse may be associated with findings such as poor eye contact, withdrawn nature, malnourishment, hygiene issues, cuts, bruises, inappropriate clothing or medication compliance issues. Did you notice any of these today or in the past 12 months?
Note: Answering Yes to one or more of questions 1 through 6 has a sensitivity of 47% and a specificity of 75% for elder abuse when compared with a blinded social work assessment. 31
© 2008 Mark J. Yaffe ( mark.yaffe{at}mcgill.ca ), Maxine Lithwick ( maxine.lithwick.cvd{at}ssss.gouv.qc.ca ), Christina Wolfson ( christina.wolfson{at}mcgill.ca ) and Taylor & Francis Ltd. Reproduced by permission of the original authors and the publisher (Taylor & Francis, www.tandfonline.com ). Additional information about the Elder Abuse Suspicion Index is available at www.mcgill.ca/familymed/research-grad/research/projects/elder
Other screening and assessment instruments for elder abuse include the Indicators of Abuse Screen, a 29-item checklist of problems that requires a two- to three-hour home visit by a trained health care provider (not necessarily a physician), which discriminated 84.4% of abuse cases and 99.2% of nonabuse cases in a validation study; 20 the Elder Assessment Instrument, a 44-item Likert-scale checklist with a sensitivity of 71% and specificity of 93% when used in the emergency department by trained nurses 32 and its updated revision, the Elder Assessment Instrument — Revised, a 51-item Likert-scale checklist; 33 and the Brief Abuse Screen for the Elderly, which contains five questions, requires less than a minute to complete and has 86%–90% agreement among trained health care workers (not necessarily physicians). 34 We were unable to find data on the sensitivity and specificity of the Brief Abuse Screen for the Elderly. With the exception of the Elder Abuse Suspicion Index, none of these instruments has been validated in the primary care setting.
The most recent recommendations from the Canadian Task Force on Preventive Health Care are from 1994, at which time the task force found poor evidence to include case-finding for elder abuse in, or to exclude it from, the periodic health examination. 35 The task force did, however, note that physicians should be alert for evidence suggestive of elder abuse that becomes apparent during history-taking and physical examination, such as positive answers to questions about the patient being forced to do things, being asked to sign documents he or she did not understand or being afraid; inconsistent histories from the patient and caregiver; long delays between injuries and seeking medical attention; and physical findings such as injuries in the shape of a weapon. Whenever possible, assessments of elder abuse should occur in private, as the presence of caregivers may hinder disclosure of abuse. The task force also suggested an advocacy approach to prevent further abuse, whereby physicians direct the older person to community resources. 35
- What evidence supports interventions to combat elder abuse?
Interventions can be categorized by the target (the abuser, the abused elderly person or the situation) (see Appendix 1, Part 4). All of the studies we identified 36 – 45 were heterogeneous and had substantial limitations, and it is therefore difficult to recommend any of the studied interventions.
The most promising model is that of multidisciplinary teams that include physicians, nurses, mental health care providers, protective services and professionals within the justice system. However, there has been only one study demonstrating a statistically significant measurable outcome for a multidisciplinary team. 45 This was a case–control study of the Los Angeles County Elder Abuse Forensic Center ( n = 287), which showed increased rates of prosecution for financial abuse with a multidisciplinary team. This study addressed only financial abuse, however, and its results cannot be extrapolated to other types of abuse that may be harder to prove in the justice system. More fundamentally, it remains unclear what should be considered an effective outcome and whether abused elderly people view prosecution in a positive way.
- How can physicians intervene in clinical practice?
Despite the lack of robust evidence to support recommendations, clinicians still need an approach to this relatively common problem. We encourage physicians to be aware of potential risk factors and clinical manifestations of elder abuse while recognizing the limitations of the research in this area. We also encourage physicians to consider using the Elder Abuse Suspicion Index ( Box 3 ) for older patients with risk factors for abuse, to discuss privately with the patient any concerns, to assess the patient’s decision-making capacity with regard to any proposed intervention and to consider referral to social service agencies or reporting to legal authorities, particularly in jurisdictions where adult protection laws mandate such reporting.
In the US, all but five states have some sort of mandatory reporting of elder abuse to adult protective services. According to the American Bar Association, however, “laws governing reporting are very diverse in content and structure and extremely challenging to categorize and explain.” 46 Adult protection laws in Canada similarly vary by province and territory. For example, Nova Scotia and Newfoundland and Labrador mandate that any person suspecting elder abuse is to report it without discriminating between capable or incapable older adults, whereas other provinces limit reporting to professional persons or have laws that vary according to whether the abused older person lives in a health care facility. 47
Although there is no comparable Canadian statement, the Department of Health for England has issued a government policy statement on safeguarding vulnerable adults, 48 which highlights six principles: empowerment (presumption of person-led decisions and informed consent), prevention (it is better to take action before harm occurs), proportionality (proportionate and least intrusive response appropriate to the risk presented), protection (support and representation for those in greatest need), partnership (local solutions through services working with their communities) and accountability (accountability and transparency in delivery of safeguarding). With these principles in mind and on the basis of our experience and review of the literature, we propose the approach outlined in Figure 1 . This approach has not been tested.
- Download figure
- Open in new tab
- Download powerpoint
Suggested approach to intervening in cases of suspected elder abuse. POA = power of attorney.
Assessment of suspected elder abuse should begin with an assessment of capacity. We believe that management strategies for elder abuse should be handled similarly to other medical treatment decisions with regard to capacity, namely whether the patient is able to understand and appreciate the consequences of the proposed treatment. If it is determined that the abused older person is capable, we suggest that the physician present his or her concerns about abuse to the patient, educate the patient about elder abuse and the tendency for it to increase in frequency and severity, and direct the patient to local resources, including day programs, home care, respite care, legal services, shelters and government-supported elder abuse consultants. In Canada, additional resources include the Advocacy Centre for the Elderly ( www.advocacycentreelderly.org ), the Canadian Network for Prevention of Elder Abuse ( www.cnpea.ca ), the Seniors Issues Unit of the Ontario Provincial Police ( www.opp.ca/ecms/index.php?id=151 ) and the Royal Canadian Mounted Police ( www.rcmp-grc.gc.ca/ccaps-spcca/elder-aine-eng.htm ). Imminent safety should be assessed and any concerns clearly communicated to the patient, including creation of an emergency safety plan. Respecting the capable older person’s autonomy should be a priority, however, and explicit permission should be sought before discussing any concerns with family members or caregivers who may be able to offer support to the older person.
In the case of an incapable older person who is experiencing abuse, we suggest identifying the person who has power of attorney and offering the same resources. Should there be concern that the person with power of attorney is not acting in the patient’s best interest or is the abuser in question, alternative strategies such as liaising with social service agencies, contacting other family members or guardianship through the Office of the Public Guardian and Trustee should be considered. An important caveat would be to ensure that the incapable patient does not have reversible medical causes of incapacity that could be addressed before seeking guardianship. All abused older adults should be offered more frequent medical follow-up.
Evidence regarding the risk factors for, assessment of and interventions to address elder abuse is limited. Although multidisciplinary teams have existed for several decades, only one study has demonstrated a measurable effect of such teams, and it was limited to financial abuse. Elder abuse is probably best considered as a syndrome, similar to the other “geriatric giants” 49 such as falls and frailty, given its complexity. 12 , 50 The best intervention strategy at this time appears to be education targeted at increasing awareness of elder abuse among health care professionals, 12 , 51 analogous to the incorporation of child abuse training into the medical school curriculum.
Future research is needed to clarify the risk factors for each type of abuse, to determine screening or case-finding thresholds, to define effective outcome measures and to test the efficacy of clinically feasible interventional approaches.
Elder abuse is common, affecting 5%–10% of older adults.
There is insufficient evidence to recommend screening all older people for elder abuse and insufficient evidence to recommend any one intervention.
However, physicians still need to address this relatively common health issue. An advocacy approach for suspected elder abuse is recommended.
Following an assessment of capacity, physicians should educate the patient about elder abuse and direct him or her to local resources, including home care and respite agencies, legal services, shelters and government-supported elder-abuse and police services.
CMAJ Podcasts: author interview at soundcloud.com/cmajpodcasts/wang-elder-abuse
Competing interests: None declared.
Disclaimer: Sharon Straus is an associate editor for the CMAJ and was not involved in the editorial decisionmaking process for this article.
This article has been peer reviewed.
Contributors: Xuyi Mimi Wang was involved in the conception and design of the review, literature search, abstract review, full-text review, data abstraction, and drafting and editing of the manuscript. Sarah Brisbin was involved in the abstract review, full-text review, data abstraction and manuscript editing. Tenneille Loo was involved in abstract review and manuscript editing. Sharon Straus was involved in the conception and design of the review, literature search and manuscript editing. All of the authors gave final approval of the version to be published and agree to act as guarantors of the work.
- Williams CS ,
- O’Brien S ,
- Acierno R ,
- Hernandez MA ,
- Amstadter AB ,
- Selwood A ,
- Livingston G
- ↵ Senior victims (65 years and older) of violent crime by sex and accused-victim relationship, Canada, 2009 . Ottawa : Statistics Canada ; modified 2012. Available: www.statcan.gc.ca/pub/85-224-x/2010000/t016-eng.htm ( accessed 2014 July 10 ).
- ↵ National Seniors Day … by the numbers . Ottawa : Statistics Canada ; 2014 . Available from: www.statcan.gc.ca/dai-quo/smr08/2014/smr08_191_2014-eng.htm#a1 ( accessed 2014 Mar. 26 ).
- Westendorp RG ,
- Lindenberg J
- Merchant ML ,
- Swagerty DL Jr . ,
- Takahashi PY ,
- Johannesen M ,
- LoGiudice D
- Hutchison B ,
- MacMillan H ,
- ↵ A global response to elder abuse and neglect: building primary health care capacity to deal with the problem worldwide: main report . Geneva : World Health Organization ; 2008 . Available: http://whqlibdoc.who.int/publications/2008/9789241563581_eng.pdf ( accessed 2013 Dec. 23 ).
- Burnage J ,
- Williams C ,
- Alexandra Hernandez-Tejada M ,
- Amstadter A ,
- Pérez-Cárceles MD ,
- Pereniguez JE ,
- Garre-Olmo J ,
- Planas-Pujol X ,
- Lopez-Pousa S ,
- Castle NG ,
- Laumann EO ,
- Leitsch SA ,
- Connolly MT ,
- Wolfson C ,
- Lithwick M ,
- Abraham I ,
- Strauss S ,
- Russell SL ,
- ↵ Canadian Task Force on the Periodic Health Examination . Periodic health examination, 1994 update: 4. Secondary prevention of elder abuse and mistreatment . CMAJ 1994 ; 151 : 1413 – 20 . OpenUrl Abstract
- Brownell P ,
- Sengstock MC ,
- Pillemer KA
- Pillemer K ,
- Drossel C ,
- Fisher JE ,
- Navarro AE ,
- Gassoumis ZD ,
- ↵ A practical guide to elder abuse and neglect law in Canada . Vancouver : Canadian Centre for Elder Law ; 2011 . Available: www.bcli.org/sites/default/files/Practical_Guide_English_Rev_JULY_2011.pdf ( accessed 2013 Dec. 23 ).
- ↵ Adult safeguarding: updated statement of government policy . London : Department of Health of England ; 2013 . Available: https://www.gov.uk/government/publications/adult-safeguarding-statement-of-government-policy-10-may-2013 ( accessed 2015 Mar. 26 ).
In this issue

- Table of Contents
- Index by author
Article tools
Thank you for your interest in spreading the word on CMAJ.
NOTE: We only request your email address so that the person you are recommending the page to knows that you wanted them to see it, and that it is not junk mail. We do not capture any email address.
Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager

- Tweet Widget
- Facebook Like
Jump to section
Related articles.
- Google Scholar
Cited By...
- The Impact of Financial Coaching on Older Adult Victims of Financial Exploitation: A Quasi-Experimental Research Study
More in this TOC Section
- Diagnosis and treatment of hyperemesis gravidarum
- Advances in the management of renal cell carcinoma
- Diagnosis and management of eosinophilic esophagitis
Similar Articles
Collections.
- Abuse (child, partner, elder)
- Family medicine, general practice, primary care
- Geriatric medicine
- Health policy
- Patient education

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Factors influencing intention to intervene in elder abuse among nursing students
Hee-jeong kim.
1 Department of Nursing, Namseoul University, Cheonan, Chungcheongnam-do, Korea
Min-Sook Seo
2 Department of Nursing, Sangji University, Wonju-si, Gangwon-do, Korea
3 Department of Nursing, Semyung University, Jecheon-si, Chungcheongbuk-do, Korea
Associated Data
The following information was supplied regarding data availability:
Raw measurements are available in the Supplemental Files .
This study aimed to identify the factors influencing the intention to intervene in elder abuse among nursing students.
A descriptive survey design was used, and questionnaires were completed by 182 nursing students. Statistical analysis was performed on the data collected, using SPSS 25.0, χ 2 -test, t -test, correlation, and regression analysis to confirm predictors of intention to intervene in elder abuse.
Awareness of abuse, legal and institutional knowledge, and attitude were positively correlated with the intention to intervene in elder abuse. Factors influencing the intention to intervene by nursing students were education courses about elder abuse, awareness of elder abuse, legal and institutional knowledge, and attitude.
The findings suggest that it is necessary to provide educational protocols for nursing students to improve their awareness and knowledge of elder abuse. Based on the findings of this study, there is a need for specific education programs and guidelines to increase the assessment of, and intervention in, elder abuse.
Introduction
In Korea, as of 2020, the population of older people, aged 65 or older, is 15.7% of the total population, and by 2040, it is predicted that 1/3 of the total population will consist of individuals aged 65 or older ( Statistics Korea, 2020 ). The increase in the older people population has caused social problems beyond individual problems. Among them, abuse occurs in one in six older people worldwide, and it is becoming a serious problem due to the increase in the number of cases, and various aspects including depression. ( Yon et al., 2017 ). Elder abuse is a concept that is influenced by the culture and values of society and includes not only physical abuse, but also emotional and sexual abuse ( Hall, Karch & Crosby, 2016 ; Lachs & Pillemer, 2015 ). According to a press release on elder abuse statistics in 2018, the number of abuse cases in Korea increased by 12.2%, from 4,622 cases in 2017 to 5,188 cases in 2018 ( Korea Institute for Health and Social Affairs, 2019 ).
In addition, according to the 2019 Elder Abuse Status Report, the number of reports of elder abuse reported by 34 regional older people protection agencies nationwide in Korea was 16,071, while the number of reports obligated to report elder abuse by mandatory reporters was only 877 ( Korea Institute for Health and Social Affairs, 2018 ). Even considering the difference between the experiences of abuse and reporting, there are few reports by persons liable to report abuse of senior citizens. There are differences in the perception of elder abuse by senior citizens who experience abuse and those who are obliged to report it.
Elder abuse is not an individual or family problem, but a grave issue that requires social intervention and response, especially by nurses, who are the first medical personnel to attend to older people. Medical institutions, home care, and visiting nursing are accessible to the target person and are responsible for observing their physical and psychological condition ( World Health Organization, 2015 ). Therefore, nurses should perform prevention and intervention tasks with an awareness of elder abuse and an attitude toward intervention. However, there were not many cases in which working nurses perceived behavior as elder abuse, and the number of reported cases was also very low, with 2.7% in 2019 and 3.4% in 2018 ( Korea Institute for Health and Social Affairs, 2019 ; Korea Institute for Health and Social Affairs, 2018 ).
The intention of intervention in elder abuse includes activities such as educating the target person regarding elder abuse so that they do not suffer from the abuse again, establishing the status of the abuse, and informing the relevant institutions to provide care ( Stark, 2012 ), which refers to the individual’s willingness to stop the abuse of the suspect condition according to the nurse’s own will ( Cho, 2014 ). Previous studies have indicated that the variables that influence the intention of medical personnel to intervene in elder abuse were their attitudes toward intervention ( Cho, 2014 ; Feng & Wu, 2005 ), abuse awareness ( Cho, 2014 ; Seong et al., 2016 ), and legal and institutional knowledge ( Ko, 2010 ). According to a study in Korea, research on elder abuse concerning nursing caregivers has been conducted, and the impact of clinical nurses’ involvement in elder abuse has been reported ( Cho, 2014 ; Oh & Kang, 2016 ), but research on elder abuse in the context of nursing students is rare. The education of undergraduate nursing students may become a future-oriented strategy for the long-term improvement of nurses’ sensitivity and knowledge regarding elder abuse, as well as to improve the rate of abuse reports ( Lee & Kim, 2018 ). Therefore, not only nurses, but also nursing students should be subject to systematic education regarding elder abuse. However, while Korea’s undergraduate nursing programs meet the learning objectives regarding the care of older people, only a small portion of elder abuse-related content is covered. If an act of abuse is not recognized, it cannot lead to a report; therefore, it is important for nursing college students, who will come across cases of elder in the future, to grasp the perception of abuse. In addition, nursing students who will be part of the reporting duty group after graduation should receive systematic education on how to both judge and recognize elder abuse, and to be informed on the reporting system. For this, it will be necessary to identify and verify factors related to the intention to report elder abuse and to develop a systematic education program to strengthen vulnerabilities in the future. In response, we conducted this study to prepare basic data for creating awareness among nursing college students toward elder abuse by investigating the perceptions, knowledge, and attitudes of nursing college students in this regard.
Purpose of research
This study aimed to identify the impact of nursing college students’ perceptions of elder abuse, legal and institutional knowledge, and attitudes regarding the intention to intervene in elder abuse, and to use it as a basis for improving awareness of elder abuse and early detection.
The specific purpose of this study is as follows:
- To identify the differences in the intention of intervention in elder abuse according to the general characteristics of nursing college students.
-To verify the awareness of elder abuse, legal and institutional knowledge, attitudes of nursing college students, and their intention to intervene.
-To identify the factors that affect the intention of nursing college students to intervene in elder abuse
Materials & Methods
Research method, 1. research design.
This study is a descriptive investigation to identify the impact of nursing college students’ perceptions of elder abuse, legal and institutional knowledge, and attitudes regarding the intention of elder abuse intervention.
2. Ethical consideration
Ethical approval (IRB No: NSU-202005-004) was obtained from the Research Ethics Committee of Namseoul University. Participants were informed that they could leave the study at any time without penalty, and all personal information was kept confidential.
3. Subjects of research
The subjects of this study were 182 nursing college students from three nursing departments in Chungcheong-do and Gangwon-do, who understood the purpose of the study and agreed to participate. Using the G*power 3.1 program, the appropriate number of samples was at least 166, based on an effect size of 0.15, a power of 95%, and a significance level of 5%.
4. Research variables
(1) perception of elder abuse..
This study used the perception of elder abuse modified by Kim & Lee (1998) and Jun & Song (1997) and used the elder abuse recognition tool developed by Lim (2001) as 38 questions ( Kim & Lee, 1998 ; Jun & Song, 1997 ; Lim, 2001 ). For the perception of elder abuse questionnaire, 38 items were rated on a 4-point Likert scale (1 = Strongly Disagree, 2 = Disagree, 3 = Agree, and 4 = Strongly Agree), that consisted of five subcategories: emotional abuse (10 items), verbal abuse (6 items), physical abuse (7 items), financial abuse (7 items), and neglect (8 items). Higher scores indicated worse elder abuse. When developing the instrument, in Lim ’s ( 2001 ) study, the tool’s reliability of subscales was emotional abuse .86, verbal abuse .79, physical abuse .84, financial abuse .89, neglect .86, and the overall reliability Cronbach’s alpha was .92. In this study, the reliability of the instrument was α .97, and the reliability of the subscales was emotional abuse .86, verbal abuse .91, physical abuse .98, financial abuse .92, neglect .86, and the overall reliability Cronbach’s alpha was .92 ( Lim, 2001 ).
(2) Legal and institutional knowledge of elder abuse.
To measure legal and institutional knowledge of elder abuse, Huh (2003) revised and supplemented the measures used in the study on factors that affect the perception and reporting behavior of child abuse reporting obligators. The original scale consists of five items, but in this study questionnaire, there were 12 items that consisted of three categories: definition of concepts and types (four items), law of reporting persons and institutions (four items), and system of reporting agency and reporting number (four items). The participants were required to answer each question with “I don’t know” and “I know.” If they answered “I know,” they would get one point. There were zero points for “I don’t know.” When the questions were added together, the score category ranged from 0 to 12. The combined score of 12 questions was the knowledge score for reporting elder abuse, and the higher the score, the higher the knowledge related to reporting. In this study, Cronbach’s alpha of the tool was .66.
(3) Elder abuse attitudes.
The attitude toward elder abuse tool was developed and used by Park, Choi & Lee (2013) in an intention to report study regarding a person liable to report child abuse, and Cho (2014) used a modified tool to suit older people. The tool consists of a total of 14 questions and is rated on a four-point Likert scale (1 = Strongly Disagree, 2 = Disagree, 3 = Agree, and 4 = Strongly Agree) that asks for the overall attitude toward intervention in elder abuse. Higher scores indicated more positive intervention behaviors. Examples of the questions include “If you report the elder abuse, appropriate measures will be taken by the reporting agency” and “If you intervene in the elder abuse, it will help them.” In Cho ’s ( 2014 ) study, Cronbach’s alpha for the tool was .77, and in this study, the Cronbach’s alpha for the tool was .68.

(4) Intention to intervene in elder abuse.
The intention to intervene in elder abuse was a comparative study of perceptions and intention to report elder abuse between nurses and older people, used by Ko (2010) as a measurement tool to recognize elder abuse in her study on “Aware and Intent to Report Abuse of Older Adults.” When asked if they would intervene in a hypothetical case with a total of 11 items, the scores for the four-point scale, where “Strong disagree” was 1 point, “Disagree” was 2 points, “Agree” was 3 points, and “Strong agree” was 4 points, were added together. Cronbach’s alpha for the tool’s reliability identified in the previous study was .79. In this study, Cronbach’s alpha of the tool was .79.
5. Data collection
The data collection period was from July 9 to October 9, 2020. Recruited via a bulletin board, data were collected from 182 college students attending nursing departments at three universities in Chungcheong-do and Gangwon-do. The application form was set up beside the bulletin board for ease of application. The researcher and trained research assistant confirmed the eligibility of the participants, they were informed of the purpose of the study, and their consent was obtained by written. The invitation included a link that enabled the questionnaire to be activated, completed, and returned electronically. The questionnaire was online and self-reported, and the participants were given a small gift to thank them for their participation. Response data were collected and stored using a questionnaire tool and subsequently exported for analysis. The questionnaire took approximately 15 min to complete.
6. Data analysis
The data collected in this study were processed using the SPSS 25.0, and the specific analysis methods were:
(1) The general characteristics of the subjects were calculated using frequency, percentage, average, and standard deviation using technical statistics, and the difference between the variables according to the general characteristics of the subjects was calculated using t-tests and F -tests.
(2) The subjects’ perception of elder abuse, legal and institutional knowledge of elder abuse, elder abuse attitude, and intention to intervene in elder abuse were analyzed by means and standard deviation using technical statistics.
(3) Pearson’s correction factors were analyzed to determine the correlation between variables.
(4) Multiple regression analysis was conducted to identify the factors affecting the intended elder abuse intervention.
Intent to intervene in elder abuse according to the general characteristics of the subject
A total of 163 women (89.3%) and 52 students (34.6%) from the fourth grade participated in this study. In this sample, 92 people (50.5%) said that they had no religion. In total, 162 respondents (88.5%) said they did not receive education on elder abuse, 179 (98.8%) said that they “agreed” with the elder abuse reporting law, and 2 (1.1%) said that they had experienced abuse. According to the analysis of the difference in the intent of the elder abuse intervention according to the general characteristics of the subject, the results indicated that education courses regarding elder abuse ( t = 3.067, p = .042), elder abuse ( t = 3.333, p = .021), elder abuse reporting ( t = 13.033, p <.001), and the need for education ( t = 5.429, p = .005), exhibited significant differences and did not differ in other variables ( Table 1 ).
Intent to intervene in elder abuse according to the general characteristics.
| Variables | Categories | n (%) | M ±SD | t/F | p |
|---|---|---|---|---|---|
| Sex | Men Women | 19(10.7) 163(89.3) | 37.21 ± 4.41 36.38 ± 4.58 | .553 | .458 |
| Grade | 2 3 4 | 52(34.1) 48(31.3) 52(34.6) | 36.36 ± 4.56 36.22 ± 4.87 36.92 ± 4.00 | 3.342 | .711 |
| Religion | Buddhism Christian Catholic No religion | 15(8.2) 56(30.8) 19(10.4) 92(50.5) | 35.86 ± 5.55 37.10 ± 4.31 35.94 ± 4.93 36.29 ± 4.50 | .576 | .632 |
| Education course about elder abuse | Has taken Not taken | 20(11.5) 162(88.5) | 38.15 ± 4.18 36.26 ± 4.58 | 3.067 | .042 |
| Elder abuse problem | Not very serious Not serious Serious Very serious | 2(1.2) 31(16.0) 99(54.9) 50(28.0) | 39.00 ± 5.65 34.22 ± 4.92 36.79 ± 4.28 37.12 ± 4.54 | 3.333 | .021 |
| Elder Abuse Reporting Act | Opposition Agree | 3(1.2) 179(98.8) | 27.33 ± 4.61 36.62 ± 4.41 | 13.033 | .000 |
| Need for education | Unnecessary Usually Need | 2(0.9) 72(38.7) 108(60.4) | 28.50 ± 9.19 35.70 ± 4.05 37.12 ± 4.64 | 5.429 | .005 |
| Experienced elder abuse | Has taken Not taken | 2(1.1) 180(98.9) | 35.50 ± 2.12 36.48 ± 4.58 | .091 | .763 |
Perception, legal and institutional knowledge, and attitude toward elder abuse and degree of intention to intervene in elder abuse
The average rating of the subject was 3.76 ±.33, out of a total of four points. Among them, the average rating of physical abuse was the highest level of recognition (3.95 ±.30), and emotional abuse was the lowest with an average rating of 3.51.40. Legal and institutional knowledge of elder abuse was 5.92 ± 2.29 points out of a total of 12, and attitudes toward elder abuse and intentions of elder abuse were 2.49 ±.33 points and 3.31 ±.41 points out of 4 points, respectively ( Table 2 ).
Perception, legal and institutional knowledge, and attitude toward elder abuse and degree of intention to intervene in elder abuse.
| Variables | M ± SD | M ± SD | Min | Max | Range |
|---|---|---|---|---|---|
| Awareness of elder abuse Psychological abuse Verbal abuse Physical abuse Financial abuse Elder neglect/ Elder dereliction | 3.76 ±.33 3.51 ±.40 3.85 ±.36 3.95 ±.30 3.79 ±.42 3.80 ±.36 | 143.00 ± 12.81 35.15 ± 4.01 23.14 ± 2.21 27.70 ± 2.15 26.58 ± 2.95 30.40 ± 2.95 | 38 10 6 7 7 8 | 152 40 24 28 28 32 | 38–152 10–40 6–24 7–28 7–28 8–32 |
| Knowledge Justice Law System | .49 ±.19 .67 ±.25 .62 ±.25 .17 ±.23 | 5.92 ± 2.29 2.71 ± 1.02 2.49 ± 1.00 0.71 ± 0.93 | 0 0 0 0 | 12 4 4 4 | 0–12 0–4 0–4 0–4 |
| Attitude | 2.49 ±.33 | 34.98 ± 4.71 | 26 | 52 | 1–56 |
| Intention of intervening in elder abuse | 3.31 ±.41 | 36.47 ± 4.56 | 22 | 44 | 11–44 |
Correlation between perceptions, legal and institutional knowledge, and attitudes toward elder abuse and intention to intervene in elder abuse
The intention to intervene showed a significant positive correlation with the perception of elder abuse ( r = .26, p = .005), legal and institutional knowledge ( r = .54, p = .046), and attitude ( r = .121, p = .004). Attitudes toward elder abuse showed a significant positive correlation with legal and institutional knowledge ( r = .15, p = .044) ( Table 3 ).
Correlation between perceptions, legal and institutional knowledge, and attitudes toward elder abuse and intention to intervene in elder abuse.
| Variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| r(p) | ||||
| Awareness of elder abuse | 1 | |||
| Knowledge | .011(.886) | 1 | ||
| Attitude | .071(.338) | .150(.044) | 1 | |
| Intention of intervening towards elder abuse | .206(.005) | .540(.046) | .121(.004) | 1 |
Factors influencing the intention of nursing college students to intervene in elder abuse
Multiple regression analyses were conducted to determine the factors affecting the intended elderly abuse intervention. In this study, we used sex as a control variable, which showed a significant difference in the general characteristics of the intentions toward elder abuse intervention. Multiple regression analysis was conducted with the three main variables of this study (elder abuse awareness, legal and institutional knowledge of elder abuse, and attitudes toward elder abuse) that were independent variables, and the intention of elder abuse intervention was a dependent variable. Testing the assumptions required for the multiple regression analyses were all satisfied. The dependent variables showed a tendency for normal distribution, and residual analysis confirmed linearity, normality, and equivalence. Furthermore, the Durbin-Watson statistic was 2.12, and there was no autocorrelation between the error terms. Next, using tolerance and variance inflation factor (VIF), the presence or absence of multicollinearity between independent variables was found to be less than 1.0 from 0.73 to 0.95, and the VIF from 1.04 to 1.36, indicating that it was below the multicollinearity criterion of 10.0.
Finally, the regression analysis showed that the regression model was significant ( F = 4.349, p = .001), representing 12.9% of the total explanatory power. The factors affecting the intent of elder abuse intervention were education on elder abuse ( β = 2.490, p = .035), awareness of elder abuse ( β = 2.479, p = .011), legal and institutional knowledge ( β =.054, p = .044), and attitude ( β =.068, p = .029), respectively. In other words, the higher the intention of nursing students to intervene in elder abuse ( Table 4 ), the higher the awareness of elder abuse, the higher the knowledge of legal and institutional knowledge, and the higher the attitude.
Factors influencing the intention of nursing college students to intervene in elder abuse.
| Predictors | B | SE | β | t | |
|---|---|---|---|---|---|
| Elder abuse awareness | 2.479 | 1.122 | .196 | 2.575 | .011 |
| Legal and institutional knowledge of elder abuse | .054 | .027 | .156 | 2.029 | .044 |
| Elder abuse attitude | .068 | .026 | .166 | 2.210 | .029 |
| Sex | .684 | .580 | .102 | 1.178 | .241 |
| Education course about elder abuse | 2.490 | 1.173 | .166 | 2.122 | .035 |
| R = .129, = 1.2, = 4.349, = .001. | |||||
This study was conducted to identify the relationship between the perception of elder abuse, legal and institutional knowledge, the attitude toward elder abuse, and the intention of elder abuse intervention, and to identify factors that affect the intention of intervention based on the results of the study. Most of the prior studies on Korean college nursing students focused on knowledge and attitudes toward older people, and there were no studies on the perception and attitude toward elder abuse and intention of intervention. It was difficult to compare the results of this study with those of the studies on nurses because of the difference in age and knowledge of nursing students, but the purpose of this study was to increase awareness of elder abuse, legal and institutional knowledge, and contribute to elder abuse intervention. Prior research has found that the perceptions of elder abuse and elder abuse were significantly related ( Ko, 2010 ; Park & Youn, 2001 ; Lee & Lee, 2007 ; Malley-Morrison, You & Mills, 2000 ). In this study, the average recognition of elder abuse was 3.76 points. This is higher than the 3.07 score of Ko’s (2010) study, which was conducted using a five-point scale targeting five general hospital nurses in 2010, and higher than the 3.56 points in Cho ’s ( 2014 ) ( Seong et al., 2016 ), where a 4-point scale was used for nurses in a senior university hospital ( Seong et al., 2016 ; Ko, 2010 ). In this study, legal and institutional knowledge was 5.92 points, and in related studies, emergency room medical personnel often did not know the actual method of reporting, even if they recognized that they had a reporting obligation ( Seong et al., 2016 ). Teaching and acquiring accurate definitions of elder abuse, screening of elder abuse, as well as relevant legal procedures and reporting methods, should be included in a future-oriented strategy to improve nurses’ sensitivity and knowledge of elder abuse, and ultimately improve reporting rates.
In this study, the attitude toward elder abuse was 2.49 points, lower than the 2.82 points of Cho ’s ( 2014 ) study ( Seong et al., 2016 ). The lower score could be explained by the study subjects being nursing students, who do not have experience in caring for older people.
Furthermore, the intention to intervene in elder abuse was 3.31 out of 4, indicating a middle or higher level. The results of the degree of abuse perception indicated that physical abuse was recognized as most severe among the various types of abuse.
Regarding emotional abuse, the severity of abuse was relatively low. It was confirmed that nursing students only recognized cases that could be clearly judged externally as elder abuse, such as physical abuse. This implies a need for education in recognizing various types of elder abuse, such as emotional, economic, neglect, and abandonment.
In this study, the perception of elder abuse, legal and institutional knowledge, elder abuse attitude, and intervention intention all revealed significant positive correlations, being consistent with the results of previous studies targeting nurses ( Ko, 2010 ; Park, Choi & Lee, 2013 ; Kim, 2010 ; Song, 2007 ). According to the regression analysis, the factors affecting the intention of intervention in elder abuse were identified as variables related to education, awareness of elder abuse, legal and institutional knowledge, and elder abuse attitudes, with an explanation of 12.9%. This was similar to the results of Cho (2014) and Park & Youn (2001) , who studied nurses’ intention to, and behavior of, reporting child abuse ( Seong et al., 2016 ; Park, Choi & Lee, 2013 ). When attitudes are formed, reactions may exist before meeting the object and affect behavior ( Erwin, 2001 ). Even in previous studies on knowledge, attitudes, and behaviors regarding older people, knowledge and attitudes influenced behavior ( Kim, Oh & Wang, 2016 ).
In Korea, nurses are already obligated to report elder abuse, and if they do not report, they are subject to legal intervention in elder abuse in terms of a fine. If this will be transmitted to the nurses, the community, and the family, the professional responsibility of the nurse to report abuse will increase along with the intervention behavior. To do this, it is necessary to advise the role of nurses as advocates for the underprivileged through education and to share awareness.
This study found that to ensure active intervention when encountering elder abuse, it is necessary to raise awareness, improve legal and institutional knowledge, and investigate attitudes toward elder abuse that affect the intention to intervene; training in geriatric nursing should hence be given. This study proposes further research on the development of educational programs for nursing students to increase their intention to intervene. It is necessary to receive a thorough education on elder abuse in order to recognize abuse cases; the development of a curriculum for this is urgently required.
As with child abuse, it is necessary to educate people on effective recognition methods elder abuse, such as education through role play, and a case-based training approach ( Kim & Lee, 2013 ). Furthermore, a specific and systematic procedure and plan should be developed to enable nursing students to easily intervene in elder abuse ( Rosen et al., 2018 ).
Conclusions
This study was conducted in the absence of research on the perceptions and attitudes of nursing college students regarding elder abuse. This study tried to identify the impact of perceptions of elder abuse, legal and institutional knowledge, and the attitude of elder abuse on the intention of intervention in elder abuse. According to this study, the variables that affect the intention of nursing college students to intervene in elder abuse were education, awareness of elder abuse, legal and institutional knowledge, and attitude. Therefore, to increase the intention of elder abuse interventions in prospective nurses, it is necessary to improve the perception of elder abuse and attitudes toward elder abuse to enhance the discovery and judgment of elder abuse cases and to improve knowledge.
The limitations of this research are as follows:
First, this study was conducted only for nursing college students attending three universities in Chungbuk and Gangwon. Therefore, it is difficult to generalize the results. Repeated studies are required for nursing students in various regions. Second, among the measurement tools used in this study, the legal and institutional knowledge and attitude tools for elder abuse are modified and need to be developed and studied in the future.
Based on the results of this study, the following suggestions are proposed. First, we propose the development and application of education programs for nursing college students to improve the intention of intervention in elder abuse. Second, we propose a tool development study that is necessary to study the intentions of elder abuse.
Supplemental Information
Supplemental information 1, supplemental information 2, supplemental information 3, funding statement.
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2020S1A5A8046754). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
The authors declare there are no competing interests.
Hee-Jeong Kim and Min-Sook Seo conceived and designed the experiments, performed the experiments, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Dahye Park conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
Ethical approval (IRB No: 1041479-HR-202005-004) was obtained from the Research Ethics Committee of Namseoul University.
- NLN Certification
- Assessment Services
- CNEA Accreditation
- NLN Foundation
- Mission & Core Values
- History & Archives
- Board of Governors
- Senior Management
- Consultants & Speakers Bureau
- NLN Nominations
- Career Center

Henry and Ertha Williams
Julia morales and lucy grey, millie larsen.
- Developing Interprofessional Education and Practice in Oral Health
- Importance of Oral-Systemic Health in Older Adults
- Performing Oral Health Assessments on Aging Patients
- Oral Health for the Older Adult Living in the Community
- Elder Abuse in the United States
- Geriatric Syndromes
- Mental Health Needs of Older Adults
- Student-Led Geriatric Nursing Conference: Evidence in Practice
- Teaching Oral Health Care for Older Adults
- Using Case Study Betsy to Understand Down's Syndrome & Dementia
- Using Cinema to Enhance Teaching Issues Related to Older Adults
- Using the Monologue of Doris Smith to Understand Situational Decision-Making
- Caring for the Caregiver
- Caring for the Older Adult at Risk for Falling
- Coordinating and Managing Care During Transitions Among Care Settings
- End-of-Life Decision Making for Older Adults: Competent and Compassionate Care
- Myths of Aging
- Using Continuing Care Retirement Communities to Enhance a Better Understanding of Older Adults
- ACE.S Knowledge Domains
- ACE.S Essential Nursing Actions
- ACE.S Framework
- ACE.S Development & History
- ACE.S Additional Resources
- ACE.S Video Library
ACE.S Unfolding Cases
An unfolding case is one that evolves over time in a manner that is unpredictable to the learner. New situations develop and are revealed with each encounter. Every ACE unfolding case uses the highly regarded unfolding case model developed for Advancing Care Excellence for Seniors (ACE.S) . Each case includes the following:
- A first-person monologue that introduces the family and the complex problems they are facing.
- Simulation scenarios designed to help students practice assessing function and expectations of their patient(s), with links to appropriate evidence-based assessment tools. Suggestions for debriefing are included.
- An innovative final assignment that asks students to finish the story .
- Instructor toolkits with suggestions on how to use the various components of the unfolding cases and incorporate them into the curriculum.
These unfolding cases combine the power of storytelling with the experiential nature of simulation scenarios. They are intended to create a robust, meaningful experience for students, one that provides a simulated experience of continuity of care and that will help them integrate the Essential Knowledge Domains and Nursing Actions into their practice of nursing. We hope you will give them a try! Standardized/Simulated patients are recommended for all ACE simulations. If you are not already familiar with the Association for Standardized Patient Educators Standards of Best Practice, we encourage you to review them.
Learn more about unfolding cases by visiting the How to Use an Unfolding Case page.
Sherman "Red" Yoder
Nln leadership development program for simulation educators project mapping the ace.s unfolding cases to the aacn essentials.
Project Disclaimer: Simulation leadership projects are a requirement for the Leadership Development Program for Simulation Educators. All projects are then placed within SIRC for the benefit of the nursing education community. Inclusion of this specific project does not constitute an endorsement by the NLN of the AACN Essentials.
Unfolding Cases with Older Adults from Other ACE Programs
Butch sampson (ace.v), eugene shaw (ace.v), ertha williams (ace.z), george palo (ace.z), judy and karen jones (ace.z), mike walker (ace+).
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Education program promoting report of elder abuse by nursing students: a pilot study
Affiliations.
- 1 Department of Nursing, Semyung University, 65 Semyung-Ro, Jechoen-Si, Chungbuk, Republic of Korea.
- 2 Department of Nursing, Dong-A University, 3 Dongdaeshin-Dong Seogu, Busan, 602-714, Republic of Korea. [email protected].
- PMID: 37003984
- PMCID: PMC10064949
- DOI: 10.1186/s12877-023-03931-0
Background: Elder abuse is an important public health concern that requires urgent attention. One main barrier to active responses to elder abuse in clinical settings is a low level of relevant knowledge among nurses. This study aims to develop an educational program to promote an intent to report elder abuse among nursing students and assess its effectiveness, with a focus on the rights of older adults.
Methods: A mixed method design was used with the Analyze, Design, Develop, Implement, and Evaluate model. Twenty-five nursing students from Chungbuk Province participated in the study. Attitude toward older adults and knowledge of, awareness of, attitude towards, and intent to report elder abuse were assessed quantitatively and analyzed using paired t-test. The feasibility of the program and feedback were collected qualitatively through group interviews and analyzed using content analysis.
Results: After the education program, attitude toward older adults (Cohen's d = 1.08), knowledge of (Cohen's d = 2.15), awareness of (Cohen's d = 1.56), attitude towards (Cohen's d = 1.85), and intent to report elder abuse (Cohen's d = 2.78) increased, confirming the positive effects of this program. Overall, all participants were satisfied with the contents and method of the program.
Conclusions: The method of program delivery should be improved and tailored strategies to boost program engagement among nursing students should be explored to implement and disseminate the program.
Keywords: ADDIE model; Education program; Elder abuse; Nursing students; RE-AIM.
© 2023. The Author(s).
PubMed Disclaimer
Conflict of interest statement
The authors declare no competing interests.
The process of participant recruitment
Similar articles
- Cinematic Virtual Reality for Educating Health Care Providers About Type 2 Diabetes, Disability, and Elder Abuse and Neglect: A Pilot Study. Beverly EA, Love C, Love M, Lammert L, Bowditch J. Beverly EA, et al. J Diabetes Sci Technol. 2023 Sep;17(5):1160-1171. doi: 10.1177/19322968231171586. Epub 2023 Apr 28. J Diabetes Sci Technol. 2023. PMID: 37114917 Free PMC article.
- Elder Abuse Education Using Standardized Patient Simulation in an Undergraduate Nursing Program. Ross MET, Bryan JL, Thomas KL, Asghar-Ali AA, Pickens SL. Ross MET, et al. J Nurs Educ. 2020 Jun 1;59(6):331-335. doi: 10.3928/01484834-20200520-06. J Nurs Educ. 2020. PMID: 32497235
- A cluster randomized trial on improving nurses' detection and management of elder abuse and neglect (I-NEED): study protocol. Loh DA, Choo WY, Hairi NN, Othman S, Mohd Hairi F, Mohd Mydin FH, Jaafar SN, Tan MP, Mohd Ali Z, Abdul Aziz S, Ramli R, Mohamad R, Lal Mohammad Z, Hassan N, Brownell P, Bulgiba A. Loh DA, et al. J Adv Nurs. 2015 Nov;71(11):2661-72. doi: 10.1111/jan.12699. Epub 2015 Jun 2. J Adv Nurs. 2015. PMID: 26031344 Clinical Trial.
- Exploring undergraduate elder abuse education in nursing: a scoping review. Natan MB, Hazanov Y. Natan MB, et al. Gerontol Geriatr Educ. 2024 Jun 9:1-15. doi: 10.1080/02701960.2024.2362749. Online ahead of print. Gerontol Geriatr Educ. 2024. PMID: 38852169 Review.
- Education and a multi-agency approach are key to addressing elder abuse. Bond C. Bond C. Prof Nurse. 2004 Dec;20(4):39-41. Prof Nurse. 2004. PMID: 15624621 Review.
- Yon Y, Ramiro-Gonzalez M, Mikton CR, Huber M, Sethi D. The prevalence of elder abuse in institutional settings: A systematic review and meta-analysis. Eur J Public Health. 2019;29(1):58–67. doi: 10.1093/eurpub/cky093. - DOI - PMC - PubMed
- Lee YJ, Kim Y, Park JI. Prevalence and factors associated with elder abuse in community-dwelling elderly in Korea: Mediation effects of social support. Psychiatry Investig. 2021;18(11):1044. doi: 10.30773/pi.2021.0156. - DOI - PMC - PubMed
- Han SD, Mosqueda L. Elder abuse in the COVID-19 era. J Am Geriatr Soc. 2020;68(7):1386–1387. doi: 10.1111/jgs.16496. - DOI - PMC - PubMed
- Ha J, Park D. Educational needs related to elder abuse among undergraduate nursing students in Korea: an importance-performance analysis. Nurse Educ Today. 2021;104:104975. doi: 10.1016/j.nedt.2021.104975. - DOI - PubMed
- MohdMydin FH, Othman S. Elder abuse and neglect intervention in the clinical setting: perceptions and barriers faced by primary care physicians in Malaysia. J Interpers Violence. 2020;35(23–24):6041–6066. doi: 10.1177/0886260517726411. - DOI - PubMed
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
MENU Elder Justice Initiative Home
- Physical Abuse
- Psychological Abuse
- Financial Exploitation
- Neglect & Abandonment
- Sexual Abuse
- Red Flags of Elder Abuse
- State Elder Abuse Flyers
- Find Help Near You
- Senior Scam Alert
- Prosecutor Training & Resources
- Federal & State Samples
- State Elder Abuse Statutes
- Law Enforcement
- Victim Specialists
- Network Locator Map
- Highlighted Networks
- MDT Resources
- MDT Webinars
- MDT Guide & Toolkit
- MDT Peer Support Listserv Community
- Guardianship
- Federally Funded Research
- Forensic Research
- Foundational Articles
- Elder Abuse Flyers
- Community Presentations
- Webinars, Training, and Events
Abuse Stories
This collection contains all stories of abuse that have been featured in the Victim, Family & Caregiver Resources: Neglect & Abandonment , Sexual Abuse , Physical Abuse , Psychological Abuse, and Financial Exploitation .
NEGLECT & ABANDONMENT
Abandonment by adult daughter.
Juliette, 87, lived with her daughter, Nanette, for the past 3 years. Nanette helped Juliette with daily activities, such as getting her meals, bathing, and cleaning the house. Nanette decided to move in with her boyfriend in another state and left her mother alone in the home. About a week later, Juliette’s niece happened to be in town and stopped by to visit her aunt. She saw that the inside of the house was in very bad condition and found Juliette in poor health. Juliette’s niece contacted Adult Protective Services (APS) and the State Area Agency on Aging.
Neglect by Daughter and Son-in-Law
Kofi, 84, was diagnosed with Alzheimer’s disease and moved in with his daughter's family. Sometimes Kofi had trouble sleeping, had physical and verbal outbursts, and began wandering. His daughter and son-in-law were afraid that Kofi might wander out of the house if they left him alone. They locked the doors to the house so that Kofi could not get out and wander around when they left for work. A neighbor noticed Kofi trying to get out of the house. She contacted the local police and Adult Protective Services (APS).
Neglect by Son and Daughter-in-Law
Tamara, 76, lived alone but had trouble getting around. Her son and his wife asked Tamara to move in with them. Tamara had her own bedroom on the second floor and stayed there most of the time. She could not use the stairs easily. Her son and daughter-in-law both traveled frequently for work and sometimes neglected to give her adequate food and water. They also failed to groom her or to clean her room consistently. One day Tamara became dizzy, weak and disoriented so her daughter took her to the hospital. The hospital staff discovered that she was dehydrated, disheveled and obviously unwashed. They asked about her care but Tamara said she was well cared for. Nevertheless, as required by law, the hospital staff reported suspected neglect to Adult Protective Services (APS).
Neglect by Sons
Clarence, 79, invited his two adult sons to move in with him so he would not be alone after his wife died. The sons soon sent Clarence out to live in the shed and locked him out of the house. Sometimes his sons put food out for him. Occasionally they gave him a basin of cold water with a washcloth. When one of Clarence’s neighbors noticed that Clarence seemed to be living in the shed, she called Adult Protective Services (APS) anonymously and reported what she had seen. She then decided Clarence may need immediate help so she called the police to do a welfare check.
Abandonment by Guardian/Conservator
Henrietta, 88, required a court appointed guardian due to combined physical and mental disabilities that left her partially incapacitated. Her niece, Roberta, was appointed as Henrietta’s guardian. Roberta visited Henrietta in her home a few times but then never came back and made no further arrangements for her care. A neighbor noticed the lack of activity at Henrietta’s house. The neighbor knocked but couldn’t get Henrietta to answer door so she called law enforcement for a welfare check and Adult Protective Services (APS).
June, 73, suffered a severe brain injury. At first she was able to care for herself but as she got worse, a court appointed Sam as her legal guardian to assist her. He saw June two times in the first six months but did not return to see June and did not arrange for her care. He falsified reports to the court stating that he saw June every three months. As a result, no one knew that June was living on her own without Sam’s help. June was unable to remember to clean her house and the trash had not been taken out in many months. Due to the deterioration of her house, June received a visit from a county health officer who discovered that June was very frail. The county health officer was a mandatory reporter and called Adult Protective Services (APS). APS petitioned the court for a new guardian.
Back to Top
SEXUAL ABUSE
Sexual abuse by nursing aide.
Margaret, 77, lived in a nursing home that was known for good residential care. One day, a nursing aide noticed that Margaret appeared anxious but Margaret would not explain why. While preparing her for a bath, the nursing aide saw multiple bruises on Margaret's arms, neck and back and asked what happened. Initially, Margaret did not say anything. Subsequently, the director of nursing learned from another resident that a new aide had sexually assaulted Margaret. As required by law, the director of nursing reported the sexual assault to Adult Protective Services (APS), and APS initiated an investigation, involving the Ombudsman and local law enforcement.
Sexual Assault by Caregiver
Eduardo, 80, had a stroke. His family hired an in-home caregiver to assist with his daily needs such as bathing and going to the toilet. One day his daughter stopped by to help see her Dad. As she helped him get dressed, he winced and she noticed that his genital area was red and irritated. Her father started to cry and mumbled something about the caregiver hurting him there. The daughter immediately called Adult Protective Services (APS) to make a report. She also called the agency where the caregiver worked, made a complaint, and ended services. APS alerted the law enforcement.
Sexual Assault by Family Member
Pearl, 70, took her nephew in when his mother could not handle his behavior problems. The nephew began viewing pornography on the TV that he shared with his aunt. Pearl was uncomfortable about this and told her nephew to stop. One day, the nephew came home and was high on drugs. He forced himself sexually upon his aunt. Pearl called 911 for local law enforcement and went to the hospital where she met with a sexual assault victim specialist.
Sexual Abuse by Guardian/Conservator
Angela, 71, required guardianship because of her continued alcohol and drug abuse. The court appointed Richard as her guardian. Soon after his appointment, he gave Angela more drugs, sexually assaulted her, and threatened her with prison for her drug use if she reported him. Angela summoned the courage to go the local police and contacted a lawyer to obtain a new guardian.
PHYSICAL ABUSE
Physical abuse by adult grandsons.
Katherine, 82, raised two grandsons, Joel and Kent. They had physically abused her since they were teenagers. After 12 years in prison, Joel returned to his grandmother's home because he had nowhere to go. One night Joel came home and was drunk. He banged on the door but Katherine told Joel to go away. After he entered the house through a back window, Joel beat his grandmother. Katherine went to a neighbor’s house and called 911. Joel was arrested and Katherine was taken to the hospital. The police contacted Adult Protective Services (APS).
Physical Abuse by Disabled Adult Son
When George, 79, lost his wife of 50 years to cancer, his son, Lawrence, came to live with him. Lawrence was on disability due to a traumatic brain injury. The brain injury caused behavior changes, including difficulty with self-control and verbal and physical outbursts. The injury also caused violent mood swings. Occasionally, Lawrence went to a neighbor's apartment and got drunk. One night when Lawrence returned home, George asked him if he was drunk. Lawrence yelled "NO" and punched his father in the face. Because George was afraid of further violence, he called 911 to get help from the police.
Physical Abuse by Spouse
After 58 years of marriage, Virgil and Ella, both 83, knew each other's habits well. Sometimes, when they argued they became physically violent. Nevertheless, they said they loved each other and had never considered divorce. Violence was unfortunately a part of their relationship. As Ella aged, she developed osteoporosis. She began to worry that if she fell down when they were fighting each other she might end up with a broken bone. She confided this to a friend, and her friend suggested calling the local domestic violence hotline to speak with a counselor.
Physical Abuse by Guardian/Conservator
Blair, 65, had no close relatives. Because of early-onset dementia, he was placed in a nursing home and required guardianship. Chris, Blair’s guardian, came to Blair’s nursing home every few months to see how Blair was doing. During the last visit, Chris began slapping Blair to wake him up. Joan, a care attendant rushed to the room when Blair began crying out for Chris to stop. Joan noticed marks on Blair’s face and asked what had happened. Blair was unable to tell Joan what had happened but Chris quickly left the room. Joan reported the incident to her supervisors who helped her make a report to Adult Protective Services (APS). The report triggered involvement by the state ombudsman and local law enforcement.
Physical Abuse by Long-Term Care Aide
Monica, 79, was placed in a long term care facility when her ALS became severe and her family could no longer care for her. Her family became concerned when they saw bruising on her arms and back. Monica was not able to speak and could not tell her family how she got the bruises. Monica’s family asked the staff about the bruising but was not satisfied with the explanation. The family also noticed that when a certain aide helped bathe her, Monica became upset and agitated. They suspected that the aide was hitting Monica and called local law enforcement.
PSYCHOLOGICAL ABUSE
Psychological abuse by daughter.
Zoe, 79, was healthy, independent and lived with her unmarried daughter, Trish, to share expenses. Zoe believed they had a good relationship. Nevertheless, Trish sometimes yelled at Zoe, calling her horrible names and telling her she was worthless. Trish began threatening to put Zoe in a nursing home. Zoe tried to ignore these rants because she was grateful to live with her daughter. However, she thought she deserved to be safe from such comments. Zoe eventually told a close friend about Trish’s yelling and threats. The friend suggested that Trish and Zoe seek counseling and that Trish get respite help from a local Agency on Aging.
Psychological and Physical Abuse by Spouse
Sarah, 75, had been married for over 50 years to Saul who was abusive. The abuse had a pattern. Her husband would start following her around watching her every move. Then he would make comments under his breath. Finally, he would start pointing his finger in her face and pushing her around. Since Saul’s retirement, this pattern seemed to be getting worse and happening more often. Sarah picked up a pamphlet on Domestic Violence at her synagogue and decided to make her first call for help. From her conversation with the domestic violence advocate, she learned about resources in her area and steps she could take to be safe.
Jane had not seen her friend Harry, 87, at Mass for weeks. This was not like her friend since Harry went to Mass almost every Sunday. Jane stopped by Harry’s house. Harry answered the door and Jane was shocked. Her friend had lost weight, looked terrible, and had obviously been crying. Harry told Jane in a hushed voice that since his daughter had moved in she would not let him go to church, the senior center, or even out of the house. Harry said that his daughter was now controlling everything including his money. Before Jane could say anything, Harry’s daughter started yelling and Harry quickly closed the door. Jane decided to make an anonymous report to Adult Protective Services (APS).
Psychological Abuse by Guardian/Conservator
Mark, 75, had Alzheimer’s disease and was beginning to have severe memory loss and trouble walking around the house. Mark’s paid caregiver, Yolanda, asked the court to appoint a guardian. Each time the guardian, Mrs. McKee, visited with Mark, she made fun of his memory problems and inability to remember where he was or even who Yolanda was. Yolanda became worried about Mark and the fact that Mrs. McKee, the court appointed guardian, did not seem to take Mark’s condition seriously. Yolanda called Adult Protective Services (APS) and the probate court to review Mark’s guardianship.
Psychological Abuse (cyber bullying) by Stranger
Rosie, 75, lived alone in an independent senior housing community. Her next door neighbor, a disabled retiree, repeatedly emailed her rude messages and sent vulgar and threatening messages to her cell phone. Fearing her neighbor might harm her if she told him to stop Rosie contacted local law enforcement, and filed criminal charges as well as a petition for a civil restraining order. She also notified housing management.
FINANCIAL EXPLOITATION
Financial Exploitation by Family, Close Friends, or Neighbors
Financial Exploitation (fraud) by Spouse
John, 68, and Bernice, 65, had a “second marriage.” John worked as an engineer and Bernice stayed home. Jointly, they had purchased 22 acres with a second home for their retirement. Trying to mend poor relationships with her sons from her first marriage, Bernice asked John to add one son to the property deed. He agreed. While John was on a business trip, Bernice faxed John the last three pages of the deed for his signature. He signed and returned the form. Unknowingly, he had signed a form deeding the entire property to Bernice who then “gifted” the property to her son. John contacted a lawyer.
Financial Exploitation (identity theft) by Adult Child
Joseph and Malvina, both 80 and retired, had taken in their daughter after her release from prison. Soon after she moved in, the couple received one credit card bill for $8,347, another for $12,694, and a third for $10,012. The couple had no idea their daughter had used their credit cards or that she had opened additional credit card accounts in her mother’s name. Now, Joseph and Malvina were faced with significant debt. The couple’s other adult child contacted Adult Protective Services (APS), the credit card company and the Federal Trade Commission (FTC).
Financial Exploitation (theft) by Guardian/Conservator
Monte, 82, had moderate dementia and required guardianship due to his worsening disease. Unfortunately, Monte had never given his only son, Samson, Power of Attorney. Monte also no longer had sufficient mental capacity to execute a power of attorney for Samson, who now lived out of state. Monte’s personal assistant, John, handled all of Monte’s financial transactions for him. Samson was concerned about John’s access to his father’s finances and reviewed Monte’s account statements while visiting his father over the summer. Samson discovered that several times John had taken over $3000 from one of Monte’s little used accounts. Samson contacted the investment firm, local law enforcement and Adult Protective Services (APS) for help.
Financial Exploitation (misuse of a power of attorney) by Relative
Russell, 88, needed help managing his day to day affairs. His nephew, Jack was out of work and offered to come and live with Russell and help him while Jack looked for a job. Jack took his uncle to the bank saying he wanted to protect Russell’s money. Russell told the bank teller to add Jack to his bank accounts. Jack then downloaded a power of attorney (POA) form from the Internet and had Russell sign it. With the POA, Russell’s credit card company added Jack as a second user to his credit card. When Russell's sister visited him, she asked about the situation. Russell told her that he thought their nephew was stealing his money. She and Russell went to the bank and learned that Jack had spent a considerable amount of his uncle’s money. The sister alerted bank officials, Adult Protective Services (APS) and local law enforcement. Russell filed for an emergency civil protective order to have Jack removed from his home.
Financial Exploitation (theft) by Friend
Ya, 84, became friends with Michelle, 72, in a computer class at the senior center. Using her own computer, Michelle established an online account to help Ya pay her bills. However, Michelle wrote checks for some of her own bills as well as for Ya’s bills. Ya was unaware that Michelle was writing checks for herself until she saw a returned check made out to a cell phone company. Ya didn’t own a cell phone. When she checked her account, Ya discovered that most of her money was gone. Ya contacted local law enforcement and asked her bank to investigate.
Financial Exploitation (promises exchanged) by Acquaintance
Barbara, 76, a retired high-ranking federal government employee, was independent and lived alone. She was recently diagnosed with Alzheimer’s disease and knew she would need more help in the future. Barbara asked Margie, a former neighbor, who was recently divorced, to move in with her. Over time, they agreed that Margie would care for Barbara in her old age and that in return, Barbara would provide Margie’s with food and housing. Barbara gave Margie her power of attorney for access to all her accounts and named her the sole beneficiary of her investment portfolio. After a several months, Barbara noticed her accounts were almost empty and called local law enforcement which also notified Adult Protective Services (APS).
Financial Exploitation by Trusted Professionals
Financial Exploitation (inappropriate products) by Investment Broker
Jackie was a successful investment broker. She had a reputation for making her clients wealthy. Recently Julio, 80, asked Jackie for financial advice. She recommended investments that had high growth potential but were risky for older adults. When Julio’s daughter reviewed his investment portfolio, she found he had investments that wouldn’t provide a return for 30 years and would do Julio little good. Julio contacted the Commodity Futures Trading Commission (CFTC) to check the background of financial professionals, the Securities and Exchange Commission ( SEC) and Adult Protective Services (APS).
Financial Exploitation (investment fraud) by Financial Advisor
Millie, 63, was a public school cafeteria worker who saved for retirement and wanted to help her grandson go to college. A friend recommended Tom, a polite, outgoing financial adviser. Millie didn’t understand the stock market but, after attending a retirement seminar, trusted Tom to invest her money. When she wanted to give her grandson money for college, Millie learned most of the money she had invested was gone. Tom had created fake account statements that showed Millie was making money. Millie contacted Tom’s company and reported him to the Attorney General and Adult Protective Services (APS) in her state.
Financial Exploitation (investment fraud) by Tax Preparer
Alex, an accountant, gave discounts for tax preparation to clients who were over age 65. He built a clientele of wealthy older single adults, widows or widowers, and found ways to get them tax refunds. Many of Alex’s clients gave him Power of Attorney; he also served as their financial adviser. Upon request, Alex gave his clients a statement of their account. Otherwise, he called clients with good news about their investments or about tax loopholes that he took advantage of for the client. When a client’s son learned the deed to his father’s house was in Alex’s name, he looked into his father’s finances and discovered Alex controlled all of his father’s assets. The client’s son contacted the Attorney General, IRS and Adult Protective Services (APS) in his father’s state.
Financial Exploitation (forgery) by Professional Caregiver
Amarjit, 91, paid his own bills. When he opened his bank statement he noticed four $150 checks had been made out to his home health aide. He knew he had not written or signed the checks. Amarjit contacted his bank and local law enforcement.
Financial Exploitation (improperly obtained power of attorney) by Professional Caregiver
Roman, 84, was bedridden. He hired Bob to provide caregiving services. Soon after, Bob forged Roman’s signature to create a fake Power of Attorney (POA) that gave Bob the power to act in Roman’s place. Using this illegal Power of Attorney, the bank allowed Bob to put his name on Roman’s savings and checking accounts. Bob explained to the bank that Roman agreed to the change but couldn’t be present because he was bedridden. Bob later put his own home address name on Roman’s accounts. Roman became concerned when he stopped receiving monthly statements from the bank. Roman contacted the bank immediately and local law enforcement.
Financial Exploitation (fraud) by Representative Payee
Carollee appeared to take good care of the older adults, including veterans, who lived in the group home where she worked. Because most of the residents were disabled and had no family to represent them, Carollee became the representative payee for their Social Security and Veteran’s Benefits. The regular postal carrier became curious when he started delivering over 30 envelopes from Social Security and Veteran’s Benefits to Carollee’s home each month. He thought she lived alone so he notified the local postal inspector through the US Postal Inspection Service hotline, Veterans Affairs, and Adult Protective Services (APS).
Financial Exploitation (inappropriate product) by Mortgage Broker
John, 68, wanted to provide for his wife, Vickie, 62, and leave money for his children when he died. He and his wife thought their home would provide this economic security after they both retired. Less than a year after his retirement, John had a massive stroke and died. Vickie contacted a mortgage broker whose ad she saw in a local magazine. The mortgage broker persuaded Vickie, who had been diagnosed with dementia, to sign a reverse mortgage on her house. Vickie’s daughter learned of the transaction and contacted local law enforcement and Vickie’s mortgage lender.
Financial Exploitation by Strangers
Financial Exploitation (internet identity theft) by Stranger
Naira, 71, was single, disabled and retired. When she got an email from her bank requesting verification of her account numbers, Naira complied. Later she opened an email that she thought was from a government official investigating Medicare fraud. The email asked her to provide her Medicare number to verify that there was no fraud on her account. When her bank manager called to confirm that she wanted to close her accounts, Naira learned the money in her savings and checking accounts was gone. She told the bank manager about the bank email and he told her that it must have been a scam. When she explained how she’d given her Medicare number after the second email, the bank manager contacted the Centers for Medicaid and Medicare, the Federal Bureau of Investigation and Adult Protective Services (APS).
Financial Exploitation (fraud) by New Sweetheart
Arturo was a popular hair stylist. He was charming and attentive to widows and older women and often asked clients who seemed well-off out to dinner. During these meals, Arturo discussed his financial woes. Some customers gave him their bank account information and put him on their accounts “just in case.” Arturo helped three of these wealthy women manage their real estate investments. Two of them even made him a joint owner of their homes. When one customer died, the executor discovered her bank and investment accounts were depleted, her home now belonged to Arturo, and heirlooms were missing. The executor contacted Adult Protective Services (APS), local law enforcement and the FBI.
Financial Exploitation (grandparent scam) by Stranger
Charlie, 82, received a phone call from a “sheriff” in New Orleans. He said Charlie’s grandson had been arrested for intoxication. To be released, the sheriff said that someone needed to pay the grandson’s fine and that his parents were not home. The sheriff told Charlie to wire money to an online address. After the money was delivered, Charlie got a call from someone he thought was his grandson saying that he needed money to get home from New Orleans. Charlie became suspicious when he asked the person claiming to be his grandson a few personal questions that he couldn’t answer. The call ended amicably. Then Charlie called a nearby Federal Bureau of Investigation field office to report the incident and filed a complaint with the FBI’s Internet Crime Complaint Center online.
Financial Exploitation (home repair scam) by Stranger
At 83, Shirley, who was a retired lawyer now lived alone after the death of her husband. It had become difficult to keep up repairs on her house. One day a handyman she’d never seen before rang her doorbell and told her the gutters on her house needed to be cleaned and that she might need a new roof. Because she didn’t have anyone else to help her with these tasks, Shirley paid him $500 to clean the gutters and an additional $10,000 as a down payment for a new roof. She never saw the handyman again. She told a neighbor what had happened and the neighbor contacted Adult Protective Services (APS), local law enforcement, and the state’s consumer protection agency within the Attorney General’s office.
Financial Exploitation (lottery scam) by Stranger
Armando, 78, was thrilled when someone from the lottery called to confirm he had won $10,000. The person on the phone said that they would send the money after Armando sent a winner's fee of $500. Thinking only about what he would do with the winnings, he wired the $500 “winner’s fee” to the address the caller provided. Because he did not receive the promised lottery winnings after a month, he contacted the Federal Trade Commission (FTC).
Elder Abuse
- Nursing Home Abuse
Personal Injury
- Wrongful Death
- Traumatic Brain Injury
- Bicycle Accidents
- Construction Site Accidents
- Fracture Injury / Broken Bones
- Back & Neck Injury
- Amputation and Limb Loss
- Permanent Paralysis
- Burn Injuries
- Vision Loss / Impairment
- San Diego Auto Accident Lawyer
- San Diego Motorcycle Accident Lawyer
- Trucking Accidents
- Boating Accidents
- Airplane & Aviation Accidents
- Bus Accidents
- Product Liability
- Sports Injury
- Types of Care Facilities
- How to Recognize and Report Elder Abuse in California
- California Ombudsman | What Is an Ombudsman & How a Long Term Care Ombudsman Can Help You
- California Elder Abuse Law | Penal Code 368 PC
- Elder Abuse Statistics | Facts & Data on Elder & Nursing Home Abuse
Practice Areas
Vehicle Accidents
We handle elder abuse and neglect cases against all types of elder care facilities including residential care facilities for the eldery, assisted living care facilities, and in home health care
FIND ALL RESOURCES YOU May need
At Berman & Riedel, LLP, we are deeply committed to protecting the dignity and well-being of the San Diego Elderly. Our Elder Abuse Resources provides a personal, compassionate, and professional approach to identifying, preventing, and addressing elder abuse. With our expert legal team by your side, you have access to essential information, and advice ensure every senior is treated with the respect and care they deserve. Trust Berman & Riedel, LLP to be your reliable legal partner in creating a safer, more supportive environment for our elders.
California Elder Abuse Law | Penal Code 368 PC | What You NEED to Know
Under California elder abuse law, it is a crime to willfully cause an elder to suffer physical or mental abuse . And though this may sound clear enough, there are a wide variety of ways either of these types of abuse can take place.
Any individual who cares for an elderly person in a nursing home or assisted living facility is bound by Penal Code 368 PC to uphold high standards of living and prevention of any type of senior abuse. If your loved one has been harmed, the offender may have committed a crime.
Table of Contents
The Basics of Penal Code 368 | California Elder Abuse Laws | 368 PC
Anyone who is aged 65 years or older is considered an elder under California elder abuse law . Under these laws, elder abuse can lead to charges in either civil or criminal court. Criminal law specifically focuses on violations of California’s Penal Code 368 PC .
Criminal abuse occurs when someone willfully allows or causes an elder to suffer. This can include the infliction of either mental suffering or physical pain on the elderly person. It is also against the law to allow or put someone in a situation where their health or well-being is in danger.

Unfortunately, there are many ways someone could harm your elderly friend or relative. They could be a caregiver who abandons or deserts the senior citizen. Someone could cause abuse by deliberately isolating the elder from getting any phone calls, guests, or other forms of communication and contact.
Physical abuse may involve injury, molestation, pain, sexual assault, unnecessary use of chemical restraints, or physical restraints. People may inflict mental suffering by causing confusion or fear through harassment, threats, or intimidating behavior. Elder abuse may also involve neglecting the elder’s food, shelter, clothing, or hygiene needs.
California elder abuse law also makes it illegal to wrongfully take the elder’s money or assets. If someone spends the elder’s money without the authority or permission to do so, they can also face disciplinary action. It is also against the law to remove the elder without the consent of the conservator.
California Elder Abuse Statute
Penal Code 368 PC includes all of the different definitions and punishments involving California elder abuse law . For example, the law states anyone who embezzled or stole the elder’s money is breaking the law if the property value is worth more than $950. If they are found guilty, they can face up to “one year county jail and $1,000 fine or state prison 2, 3 or 4 years.”
What is the penalty for elder abuse in California?
The entire list of violations is covered in section b, c, d and e of Penal Code 368 PC. Ultimately, the penalty involved depends on the level of crime committed by the individual.
Section b of the penal code involves inflicting mental suffering or physical pain on an elder. It is against the law for someone to cause or allow conditions likely to cause serious bodily harm or death. When someone does this, they can get a year in jail with a $6,000 fine or be sent to state prison for two to four years.
If the elder suffered from great bodily injury, then the offender can go to jail for three years in cases where the victim is younger than 70. When the victim is 70 years old or older, the suspect can get sent to prison for five years . Meanwhile, the death of the victim can lead to five to seven years in state prison depending on whether the victim is younger than 70 or not.

Section c covers the same kinds of injuries but includes the circumstances that aren’t likely to cause great bodily harm or death. In this case, the crime is classified as a misdemeanor.
Section d and e are both California financial elder abuse laws. In Section d, the law revolves around someone other than the caretaker stealing or embezzling the elder’s property without their knowledge. Section e involves the same kind of violation, but it focuses on caretakers only.
In Section d, the violator can end up in state jail for a year with a $1,000 fine or in state prison for two to four years. If the value of the property is less than $950, then the person can end up getting a $1,000 fine and a year spent in county jail. For caretakers, the potential punishments are the same.
Is elderly abuse a felony?
It depends on if the individual harms the individual physically, mentally or financially and the extent of the harm. For example, California financial elder abuse laws allow a caretaker to be charged with a misdemeanor or felony for embezzling or stealing from the elder.
How to Bring an Action Against Someone Suspected of California Elder Abuse
If you think your family member, friend, or neighbor is a victim of elder abuse or neglect, it is essential that you report it . Elder abuse reporting laws require you to disclose your suspicions to the proper authorities. Today, Assembly Bill 1690 and Assembly Bill 1499 require staff members at elder care facilities to be trained in how to report elder abuse.
Anyone who has full-time or intermittent care for an elder is considered a mandated reporter. If you see a situation that appears to involve abuse or neglect of some kind, you are legally required to report it. Otherwise, you would be violating the California elder abuse mandated reporting laws by looking the other way or keeping it to yourself.
California Adult Protective Services
But in addition to it being the law, reporting elder abuse in California is the right thing to do. If not reported, elder abuse will often continue and escalate to a stage, sometimes even ending with dire consequences. It is always better to err on the side of caution than potentially overlook a potential case of abuse.
Whenever you come across an elder who needs immediate medical care, you should immediately call 9-1-1. Afterward, you can take the next step in reporting elder abuse to California’s Adult Protective Services (APS).
Contacting Adult Protective Services in California
Each county where you need to report California elder abuse will have a different APS office and phone number. These hotlines will help you report any incidents of abuse or neglect and get the help your loved one needs.
- Alameda County: (866) 225-5277
- San Mateo County: (800) 675-8437
- Contra Costa County: (877) 839-4337
- Santa Clara County: (800) 414-2002
- Marin County: (415) 473-2774
- Santa Cruz County: (866) 580-4357
- Napa County: (888) 619-6913
- Solano County: (800) 850-0012
- San Francisco County: (800) 814-0009
- Sonoma County: (800) 667-0404
Report to the California Department of Social Services
Occasionally, people may notice California elder abuse involving in-home care support services. For these cases, you can reach the state's Department of Social Services IHSS Fraud Hotline at (800) 822-6222 . If you prefer, you can make this report anonymously via email or phone.

When the case involves Medi-Cal or Medicare, the Bureau of Medi-Cal Fraud & Elder Abuse Hotline will be the ones to contact. You can reach them at (800) 722-0432 . They also offer the option to submit a complaint online .
Each county also has a California ombudsman who is responsible for helping people who are suffering from elder abuse. They provide education and assist in recognizing scenarios where there are signs of elder abuse or neglect .
What Happens Next: Fines & Penalties When They’re Convicted
After you report the case to the proper authorities, the case will be opened and investigated. Then, if found guilty, based on their crimes the culprit will be charged with committing a misdemeanor or a felony . If they are convicted, they may face multiple years in prison, as well as monetary fines.
The individual’s custodial sentence can range from a year in county jail to seven years in state prison. Penal Code 368 PC also includes fines ranging from $1,000 to $6,000. The exact fine or custodial sentence depends on how the elder was harmed and the extent of the injury.
California elder abuse law also includes a timeframe in which you can file in civil court. With the California elder abuse statute of limitations, you have two years to file in court . There is an exception to this rule in cases of physical or mental incapacitation and when injuries don’t manifest until after the fact.
Keep in mind, financial crimes have a different statute of limitations in California. Once the financial abuse was discovered or ought to have been discovered, you have four years to file in civil court. If you file before the statute of limitations is up, you may be able to collect damages if the other party is convicted.
Protect Your Loved Ones From Abuse
By reporting potential abuse or neglect, you could save someone’s life. California elder abuse law and Penal Code 368 PC are designed to protect loved ones from physical, mental, or financial harm . When you report potential abuse, you are giving an aging adult a better chance of getting out of their negative situation.
If you or your loved one are experiencing elder abuse, help is available. Please call our offices at (858) 240-9340 or complete the form on this page for a free evaluation.
Elder Abuse Laws | Criminal Guide
| Code Section | Description | Penalty |
|---|---|---|
| (Murder) | ||
| (Rape) | ||
| (Lewd or Lascivious Acts) | | |
| (Sexual Penetration) | ||
| (Causes or permits infliction of physical pain or mental suffering on elder or dependent adult under circumstances or conditions likely to produce great bodily harm or death) | ||
| (Causes or permits infliction of physical pain or mental suffering on elder or dependent adult under circumstances or conditions not likely to produce great bodily harm or death) | li>Unjustifiable physical pain or mental suffering | |
| (Violates provision of law proscribing theft or embezzlement - not a caretaker) | ||
| (Violates provision of law proscribing theft or embezzlement - caretaker) | ||
| (Elements of Offense - Willfully threatens to commit a crime which will result in death or great bodily injury) | ||
| (Violations, Penalties Relating to Operation or Maintenance of Long-Term Healthcare Facilities) | ||
| (Mandated Reporters of Abuse) |
Penal Code 368 PC
Penal code - pen, part 1. of crimes and punishments [25 - 680].
( Part 1 enacted 1872. )
TITLE 9. OF CRIMES AGAINST THE PERSON INVOLVING SEXUAL ASSAULT, AND CRIMES AGAINST PUBLIC DECENCY AND GOOD MORALS [261 - 368.5]
( Heading of Title 9 amended by Stats. 1982, Ch. 1111, Sec. 2. )
CHAPTER 13. Crimes Against Elders, Dependent Adults, and Persons with Disabilities [368 - 368.7]
( Chapter 13 heading added by Stats. 2010, Ch. 617, Sec. 2. )
[bg_collapse view="button-green" color="#ffffff" icon="arrow" expand_text="Show More" collapse_text="Show Less" custom_class="showhide-btn1" ]
(a) The Legislature finds and declares that elders, adults whose physical or mental disabilities or other limitations restrict their ability to carry out normal activities or to protect their rights, and adults admitted as inpatients to a 24-hour health facility deserve special consideration and protection.
(b) (1) A person who knows or reasonably should know that a person is an elder or dependent adult and who, under circumstances or conditions likely to produce great bodily harm or death, willfully causes or permits any elder or dependent adult to suffer, or inflicts thereon unjustifiable physical pain or mental suffering, or having the care or custody of any elder or dependent adult, willfully causes or permits the person or health of the elder or dependent adult to be injured, or willfully causes or permits the elder or dependent adult to be placed in a situation in which his or her person or health is endangered, is punishable by imprisonment in a county jail not exceeding one year, or by a fine not to exceed six thousand dollars ($6,000), or by both that fine and imprisonment, or by imprisonment in the state prison for two, three, or four years.
(2) If, in the commission of an offense described in paragraph (1), the victim suffers great bodily injury, as defined in Section 12022.7, the defendant shall receive an additional term in the state prison as follows:
(A) Three years if the victim is under 70 years of age.
(B) Five years if the victim is 70 years of age or older.
(3) If, in the commission of an offense described in paragraph (1), the defendant proximately causes the death of the victim, the defendant shall receive an additional term in the state prison as follows:
(A) Five years if the victim is under 70 years of age.
(B) Seven years if the victim is 70 years of age or older.
(c) A person who knows or reasonably should know that a person is an elder or dependent adult and who, under circumstances or conditions other than those likely to produce great bodily harm or death, willfully causes or permits any elder or dependent adult to suffer, or inflicts thereon unjustifiable physical pain or mental suffering, or having the care or custody of any elder or dependent adult, willfully causes or permits the person or health of the elder or dependent adult to be injured or willfully causes or permits the elder or dependent adult to be placed in a situation in which his or her person or health may be endangered, is guilty of a misdemeanor. A second or subsequent violation of this subdivision is punishable by a fine not to exceed two thousand dollars ($2,000), or by imprisonment in a county jail not to exceed one year, or by both that fine and imprisonment.
(d) A person who is not a caretaker who violates any provision of law proscribing theft, embezzlement, forgery, or fraud, or who violates Section 530.5 proscribing identity theft, with respect to the property or personal identifying information of an elder or a dependent adult, and who knows or reasonably should know that the victim is an elder or a dependent adult, is punishable as follows:
(1) By a fine not exceeding two thousand five hundred dollars ($2,500), or by imprisonment in a county jail not exceeding one year, or by both that fine and imprisonment, or by a fine not exceeding ten thousand dollars ($10,000), or by imprisonment pursuant to subdivision (h) of Section 1170 for two, three, or four years, or by both that fine and imprisonment, when the moneys, labor, goods, services, or real or personal property taken or obtained is of a value exceeding nine hundred fifty dollars ($950).
(2) By a fine not exceeding one thousand dollars ($1,000), by imprisonment in a county jail not exceeding one year, or by both that fine and imprisonment, when the moneys, labor, goods, services, or real or personal property taken or obtained is of a value not exceeding nine hundred fifty dollars ($950).
(e) A caretaker of an elder or a dependent adult who violates any provision of law proscribing theft, embezzlement, forgery, or fraud, or who violates Section 530.5 proscribing identity theft, with respect to the property or personal identifying information of that elder or dependent adult, is punishable as follows:
(f) A person who commits the false imprisonment of an elder or a dependent adult by the use of violence, menace, fraud, or deceit is punishable by imprisonment pursuant to subdivision (h) of Section 1170 for two, three, or four years.
(g) As used in this section, “elder” means a person who is 65 years of age or older.
(h) As used in this section, “dependent adult” means a person, regardless of whether the person lives independently, who is between the ages of 18 and 64, who has physical or mental limitations which restrict his or her ability to carry out normal activities or to protect his or her rights, including, but not limited to, persons who have physical or developmental disabilities or whose physical or mental abilities have diminished because of age. “Dependent adult” includes a person between the ages of 18 and 64 who is admitted as an inpatient to a 24-hour health facility, as defined in Sections 1250, 1250.2, and 1250.3 of the Health and Safety Code.
(i) As used in this section, “caretaker” means a person who has the care, custody, or control of, or who stands in a position of trust with, an elder or a dependent adult.
(j) Nothing in this section shall preclude prosecution under both this section and Section 187 or 12022.7 or any other provision of law. However, a person shall not receive an additional term of imprisonment under both paragraphs (2) and (3) of subdivision (b) for a single offense, nor shall a person receive an additional term of imprisonment under both Section 12022.7 and paragraph (2) or (3) of subdivision (b) for a single offense.
(k) In any case in which a person is convicted of violating these provisions, the court may require him or her to receive appropriate counseling as a condition of probation. A defendant ordered to be placed in a counseling program shall be responsible for paying the expense of his or her participation in the counseling program as determined by the court. The court shall take into consideration the ability of the defendant to pay, and no defendant shall be denied probation because of his or her inability to pay.
(l) Upon conviction for a violation of subdivision (b), (c), (d), (e), or (f), the sentencing court shall also consider issuing an order restraining the defendant from any contact with the victim, which may be valid for up to 10 years, as determined by the court. It is the intent of the Legislature that the length of any restraining order be based upon the seriousness of the facts before the court, the probability of future violations, and the safety of the victim and his or her immediate family. This protective order may be issued by the court whether the defendant is sentenced to state prison or county jail, or if imposition of sentence is suspended and the defendant is placed on probation.
(Amended by Stats. 2018, Ch. 70, Sec. 3. (AB 1934) Effective January 1, 2019.)
[/bg_collapse]
5 Star Rated Injury Lawyers In California

FREE CONSULTATION.
Speak directly with a partner now..
NOTE: All Fields Required
- Name * First Last
- Describe your case *
- Hidden How would you like to be contacted? * How would you like to be contacted? Phone Email
- Comments This field is for validation purposes and should be left unchanged.
Watch What Our Clients Have To Say
Elder neglect by healthcare corporation.
Wrongful Death at a California Nursing Home
Wrongful Death Legal Services
Serious Injury at Skilled Nursing Facility
Are You Ready To Speak To An Attorney on Our Team?
In the news, nursing home elopement – dementia wandering behavior & nursing home negligence, medication errors in nursing homes – a common and dangerous form of nursing home negligence, can you get a concussion without hitting your head – dispelling common concussion myths, frequently asked questions, how much does it cost to hire a personal injury attorney, can you tell me how much my case is worth.
There is no way to determine the exact value of a personal injury case, especially early in your case. However, an experienced attorney can give you an estimated range based on their experience with similar cases.
There are many factors that may influence the value of your case, such as:
- Your total financial or economic damages
- The severity of your injuries
- The impact of your injuries on your daily life
- The strength of your case
- Whether you share fault for your accident
- Insurance policy limits
Some damages are easy to calculate, such as lost wages and medical bills. Calculating the value of diminished earnings for the rest of your life or future medical needs; however, may require the help of experts. Non-economic damages like pain and suffering have no intrinsic financial value. These damages are challenging to calculate.
If your case goes before a jury, you may potentially be able to recover more than you could through a settlement. However, this introduces a new element of risk: the jury. The circumstances of your accident and even how sympathetic you or the defendant are can influence the outcome.
During your consultation, and throughout your case, we will help you understand how these factors influence your case. We will also work tirelessly to document the value of all your damages and pursue maximum compensation on your behalf.
Will My Case Go to Trial?
How do i know if i need a personal injury lawyer, do you accept cases outside of san diego.
- Name This field is for validation purposes and should be left unchanged.
Trusted By California To Handle Elder Abuse & Neglect, Serious Personal Injury, & Wrongful Death Litigation

Our Location

Our Practice Areas
- Vision Loss & Impairment
- Fractures & Broken Bones
- Spinal Cord, Back & Neck Injury
Our Practice Areas 2
Elder Abuse & Neglect
- Nursing Home Abuse & Neglect
- Bedsore Cases
- Fall Injury Cases
- Malnutrition / Dehydration
- Violation of Nursing Home Residents’ Rights
- Car Accidents
- Motorcycle Accidents
- Airplane & Aviation Accidents
This website is intended to assist affiliated healthcare professional of Stanford University Medical Center and the surrounding community with questions and management about suspected elder and dependent adult abuse.
Definition of Elder/Dependent Adult Abuse
Elder abuse can be divided into three main categories - 1. abuse/neglect by another at home, 2. at an institution, or 3. self neglect. Elder abuse refers to an act or omission that results in harm or potential harm to the health or welfare of a person age 65 or older. It can include:
- neglect (intentional or unintentional)
- abandonment
- physical abuse - including excessive medical or physical restraint, or withholding of medication, including pain medication
- sexual abuse
- financial abuse
- violation of rights - including abduction and isolation
- psychological abuse
State law on elder abuse often couples it with dependent adult abuse. A dependent adult is someone 18-64 who has physical or mental limitations that restrict his or her ability to carry out normal activities, or to protect his or her rights.
Two factors that may make an older or dependent adult more vulnerable to abuse are social isolation and mental impairment . However, in some situations, living with a caregiver or friend may increase the chances for abuse to occur. Medical visits in a safe and private environment may be the only opportunity for the patient to tell someone about the abuse.
In this website you will find out how to screen for, observe, document, and report suspected elder or dependent adult abuse.
DO YOU HAVE AN IMMEDIATE PROBLEM?
Social Work SHC 3-5091
Security 3-7222
Risk Management 3-6824
Stanford Geriatric Health Services 5-2664
Palo Alto Police (650) 329-2413
Report Elder/ Dependent Adult Abuse (800) 414-2002 for Santa Clara County
Report Long Term Care Facility Abuse (800) 231-4024
SEXUAL ASSAULT
If sexual assault is involved or suspected, do NOT do a pelvic exam. When you report to police or APS, they will make arrangements for forensic examination and counseling by SART (Sexual Assault Response Team) professionals. The Santa Clara County SART location is at Valley Medical Center.
RELATED SITES
Domestic Abuse
Child Abuse
Human Trafficking
- 415.750.4111

- Abuse, Neglect & Exploitation , Aging , Caregiving , Finances
Reporting Elder Abuse in California: What to Do If You Suspect Mistreatment or Neglect
When Tasha realized that her uncle had been stealing his mother’s money for years—small amounts at a time that had been getting bigger—she says she felt paralyzed by the shock of it. Lee had offered to manage his mother’s bills and other finances, and the rest of the family trusted that everything was taken care of. Tasha could hear her uncle’s voice in her head if she were to ask him about it: “I think my mom wants me to have some compensation for all the time I spend. It’s not really a big deal. I’m going to inherit a lot of it anyway.” But the financial limitations were starting to show in her grandma’s accounts and budgets. Tasha was worried that if she approached Lee directly, he might cause his mother further harm by pressuring her to lie about what had been going on or by making her think she’d forgotten a prior agreement they’d made about it. Tasha found herself in a position that is not so uncommon. Cases of financial exploitation and other forms of elder abuse have found a way into our society and must be remedied—both on a case-by-case basis and on the larger-scale level of public policy and through our collective understanding of older adults’ unconditional value and rights to fair treatment . Sometimes elder abuse happens at the hands of family members, friends, and caregivers who are very close to the older adult in harm’s way. And, as Tasha discovered, it can be really difficult to overcome doubts and insecurities to take action and report unacceptable abuse happening right at home. Other times, elder abuse happens under the influence of strangers, such as professional scammers, lawyers, bankers or insurance agents, who take advantage of an aging adult’s vulnerabilities. In any case, if you are a caregiver—formal or informal—for an older adult, reporting elder abuse in California is a mandatory civic responsibility , and it is indispensable for our commitment to equality without the threat of victimization and mistreatment. And, it’s important to remember that Adult Protective Services (APS) seeks to find the least restrictive option to deal with the protective issue.
In California and in General, Reporting Elder Abuse Is the Right Thing to Do
Knowing when to report perceived elder abuse can seem difficult to be absolutely sure of. You may feel as if the guidelines are subjective, especially when family members are involved in the potential abuse. But remember that everyone’s right to fair treatment and a life free from abuse and neglect is not subjective. If you become aware of or even suspect elder abuse or neglect, it’s always good to reach out through the proper channels and ensure that the older adult does not continue to be put in harm’s way. You can refer to our guides about how to recognize:
- Different forms of elder abuse
- Signs of domestic and family elder abuse
- Serious self-neglect in older adults
- Signs of physical elder abuse
- Emotional and psychological elder abuse
- Financial elder abuse among family members
- Cultural financial abuse scams that may be preying on an aging loved one
If you still have doubts, it’s always better to get some professional advice than to continue as if nothing were amiss because, in that case, you may be enabling abuse and an aging loved one’s unnecessary suffering. Read on for more information about reporting elder abuse in California. Also, know that APS is happy to consult with you. One of the benefits of contacting agencies such as APS is that they are aware of the many resources in the community that might fit your needs to help remedy the protective issue at hand.
How Can You Report Elder Abuse in California?
The California Department of Justice reminds us that “Abuse can continue and often escalates if there is no intervention. Known or suspected cases of abuse should be reported to the appropriate agencies in your area. When in doubt, err on the side of caution and report.” If you find that an older adult is in need of immediate medical care, call 9-1-1 right away; get them the direct care they need, then proceed with reporting the related elder abuse. When it comes to reporting elder abuse and neglect in California, your action steps will vary slightly if the aging adult was subject to mistreatment in the long-term care facility where they reside or if it occurred in circumstances unrelated to a residential facility. For any and all cases, an important early step is to contact APS. If you witness elder abuse or suspect that abuse or neglect may be happening, no matter the particular circumstances, determine the number of your California county’s elder abuse hotline and make the call. You can do this by referring to the Bay Area counties listed below, or if you don’t see your county listed, find the local APS contact information here .
In addition to calling California APS, if your aging loved one has experienced abuse or neglect in connection with a care facility, you should also make a report with your local county Long-Term Care Ombudsman. The toll-free 24-hour crisis line is a good place to start: (800) 231-4024. And you can get in contact with your local ombudsman program through this county directory at the California Department of Aging . If the elder abuse you perceive is suspicious activity related to In-Home Supportive Services (IHSS), you may also want to contact the California Department of Health Care Services IHSS Fraud Hotline at (800) 822-6222; you can make your report anonymously over the phone or by email. If the elder abuse or exploitation you observe is in relation to Medicare or Medi-Cal services, reach out to the Bureau of Medi-Cal Fraud & Elder Abuse Hotline at (800) 722-0432. There is also an elder abuse reporting form you can fill out online regarding Medi-Cal Fraud or elder abuse. By reaching out and giving the details of elder abuse or neglect that you’ve observed, you are giving an aging adult in crisis their best chance of recovery and safety from the threat of future mistreatment. That individual’s right to a life free from fear and unnecessary suffering is invaluable and unconditional. So, whether the injustice has been happening within the family or by strangers—whether the harm has been physical, emotional, material, or some combination of these—you hold the important responsibility to report what you know or suspect. Your actions could be the turning point for an aging loved one’s condition of life or perhaps life itself. If you have any further questions about what constitutes elder abuse or neglect or how you should go about reporting a specific case, get in touch with Institute on Aging . We are ready to help answer your questions and connect you with helpful programs and services.
Institute on Aging
Enrichment center at the presidio, related posts.

Remembering Dr. Patrick Arbore

Mental Health Awareness Roundup: San Francisco officials push for universal mental healthcare

Mental Health Awareness Month: Signs to look for and a few selfcare tips

Fall risk is higher for those with cognitive impairment

Natural light can make a world of difference for dementia patients
🌷 Happy Women`s Equality Day! 🌷 Today, we salute the inspiring women shaping a better future in aging and healthcare. Let`s honor their achievements and continue the push for equality. #WomensEqualityDay #Empowerment #InstituteOnAging

Join our United Health Equity in Aging Summit Watch Party! 📺🎉 Where: Weinberg Auditorium, 3575 Geary Blvd, San Francisco, CA When: September 18th, 2024 | 9am-4pm - Drop in anytime! Institute on Aging and @thescanfndtn invite you to a live viewing of the 2nd Annual United for Health Equity in Aging Summit. Come enjoy sessions focusing on: Elevating older adults` voices 🗣️ Innovative aging solutions ✨ Breaking down health equity barriers 🚫 Light bites and beverages provided, along with raffle and giveaway prizes! Whether you come for a bit or stay all day, we can`t wait to see you! Visit the link in our bio to RSVP today! #HealthEquitySummit #InstituteOnAging #WatchParty #CommunityEvent
We`re celebrating the incredible members of our Friendship Line team! These fantastic volunteers dedicate their time and hearts to serving our community, offering support and companionship to those who need it most. 📞💕 We recently honored these selfless individuals for their commitment and passion. Join us in applauding their amazing work and learn how you too can make a difference by visiting the link in our bio. #FriendshipLine #CommunityHeroes #VolunteerAppreciation #MakeADifference #JoinUs
Connection is just a call away! Institute on Aging`s Friendship Line understands the importance of human touch and the warmth of a friendly chat. You`re always greeted by a real person ready to listen, share a laugh, or offer support. Dial 1(888) 670-1360 and make a new friend today. Because at IOA, we believe no one should feel alone. #FriendshipLine #Friendship #InstituteonAging #WarmLine #CallUsToday
CONNECT With Us
Call ioa connect.

3575 Geary Boulevard | San Francisco, CA 94118
Phone: (415) 750 – 4111 | Fax: (415) 750 – 5338
Locations Served
Marin County | San Mateo County | Santa Clara County | Alameda County | Contra Costa County | San Bernardino & Riverside Counties
©2024 All Rights Reserved

COMMENTS
The study included nursing students who were enrolled for Diploma and BSN program, exposed to online learning, and second, third, and fourth year nursing students. ... But in case of practical, like IV infusion, it was very easy to watch the procedure in a virtual platform, but it was very difficult to perform. I feel offline clinical exposure ...
This case study reviews the use of forensic anthropology in the investigation of elder abuse. The objectives of this article are to (1) review the minimal literature related to elder abuse in the forensic anthropology and bioarchaeological record, highlighting the importance of the healing continuum and pathological influences; (2) outline the theoretical frameworks that can be applied to ...
Nursing students experienced various types of bullying and abuse in their practice areas. This study aims to assess the incidence, nature, and types of bullying and harassment experienced by Jordanian nursing students in clinical areas. A cross-sectional, descriptive design was used, utilizing a self-report questionnaire. A convenient sampling technique was used to approach nursing students ...
The participants in this study noted that bullying and lateral violence could also have implications for the victim's personal life and family. Moreover, the reputation of the ward and the nursing profession can be tarnished; the phenomenon is seen as an epidemic that adversely affects the entire team.
On 9 August 2024, Moumita Debnath, a trainee doctor at R. G. Kar Medical College in Kolkata, West Bengal, India, was raped and murdered in a college building.Her body was found in a seminar room on campus. The incident has amplified debate about the safety of women and doctors in India, and has sparked significant outrage, nationwide and international protests, and demands for a thorough ...
ELDER ABUSE SCENARIOS FOR NURSING STUDENTS. 1) A 75‐year old man with pulmonary fibrosis is admitted for pneumonia. As you are going towards his room to give him his medications, you hear his partner say to him in a nasty tone of voice: "Stop being so stubborn. I need you to give me access to your bank accounts.
This study aims to develop an educational program to promote an intent to report elder abuse among nursing students and assess its effectiveness, with a focus on the rights of older adults. ... Regarding intervening in an elder abuse case, 12 participants stated that they would only report the incident before the education, while 4 stated that ...
At home in the community—this is the most common setting. As only 5% of the U.S. elderly population reside in nursing homes at any given time, the vast majority of elders are community-dwelling. Unlike children, elders and their caregivers often become isolated, and there are few protective measures in place to watch out for them.
Background Elder abuse is an important public health concern that requires urgent attention. One main barrier to active responses to elder abuse in clinical settings is a low level of relevant knowledge among nurses. This study aims to develop an educational program to promote an intent to report elder abuse among nursing students and assess its effectiveness, with a focus on the rights of ...
Although there is a lack of concrete data, recent reports suggest that elder abuse is common. It is believed that elder abuse is more likely to occur with nursing home residents than with older adults living in community settings. In fact, 2 in 3 nursing home staff members admitted to abusing or neglecting residents in the 2020 WHO report.
Despite government efforts, elder abuse in nursing homes continues to remain a major problem . The main types of abuse in nursing homes are as follows: physical abuse (29%), resident-to-resident abuse (22%), gross neglect (14%), financial abuse (7%), and sexual abuse (7%) . A study conducted by Hawes et al. found that 40% of the staff in their ...
The strategy enhances the student's human flourishing and nursing judgment. Have students watch the video . An Age for Justice: Confronting Elder Abuse in America. This activity can take place in lecture, seminar, or in pre or post conference for clinical. Have students read the Red Flags of Elder Abuse page from the US Department of Justice.
Elder Abuse in the United States; Geriatric Syndromes; Mental Health Needs of Older Adults; Student-Led Geriatric Nursing Conference: Evidence in Practice; Teaching Oral Health Care for Older Adults; Using Case Study Betsy to Understand Down's Syndrome & Dementia; Using Cinema to Enhance Teaching Issues Related to Older Adults
To allow students to engage in a realistic case-based scenario ... was utilized for this study and included 85 nursing students and 58 physical therapy students. The students had completed didactic courses for geriatric patient care including the recognition and reporting of elder abuse. All students participate in interprofessional simulations ...
Participants noted that elderly's dependency on caregiver had high risk in occurrence of Elderly Abuse (EA) especially in case alcohol and drug dependency. There was slight decrease in score from 1 month to 3 month which suggest that continuing education is required. Cross-Sectional studies: 324 nursing students
Elder abuse is increasingly recognized as an important problem associated with significantly increased rates of hospital admission,1 nursing home placement2 and mortality.3 Estimates of prevalence vary widely, but recent studies, including a 2008 systematic review, have suggested that 5%-10% of older adults report experiencing abuse.4, 5 In December 2012, the Canadian Parliament passed Bill ...
The intention to intervene in elder abuse was a comparative study of perceptions and intention to report elder abuse between nurses and older people, used by Ko (2010) as a measurement tool to recognize elder abuse in her study on "Aware and Intent to Report Abuse of Older Adults." When asked if they would intervene in a hypothetical case ...
Abstract. Aim: The aim of this study is to investigate student nurses' perception, knowledge and awareness of elder abuse. Background: It is evidential that elder abuse tends to be unrecognized and is often hidden from public awareness. Nurses who work with older people are expected to be knowledgeable of the causes and detection of elder abuse.
ACE.S Unfolding Cases. An unfolding case is one that evolves over time in a manner that is unpredictable to the learner. New situations develop and are revealed with each encounter. Every ACE unfolding case uses the highly regarded unfolding case model developed for Advancing Care Excellence for Seniors (ACE.S). Each case includes the following:
Community Case: Suspicion of Elder Abuse Case Part 1. Growth in the aging population presents multiple opportunities for nurses to advocate for the needs of elders in communities. Judy Prescott, a home health nurse, has regularly visited Florence Brown, a 67-year-old client who experienced a myocardial infarction 6 months ago.
This study aims to develop an educational program to promote an intent to report elder abuse among nursing students and assess its effectiveness, with a focus on the rights of older adults. Methods: A mixed method design was used with the Analyze, Design, Develop, Implement, and Evaluate model. Twenty-five nursing students from Chungbuk ...
Sexual Abuse by Nursing Aide. Margaret, 77, lived in a nursing home that was known for good residential care. One day, a nursing aide noticed that Margaret appeared anxious but Margaret would not explain why. While preparing her for a bath, the nursing aide saw multiple bruises on Margaret's arms, neck and back and asked what happened.
this is a case study on elder abuse. enjoy elder adult clinical dilemma activity john peterson, 82 years old primary concept interpersonal violence ... Students also viewed. ... Study Guide Population Health Nursing exam 3; Related documents. Pre-test questions and practice; Huang PET3361 002 21264 SP16 - Online L; Study Guides for Quiz 1 and ...
In a survey of more than 4000 older people in New York State, the rate of elder abuse was found to be 7.6% 16,17; in a national survey by Laumann et al., the rate was 9%, 12 and in a national ...
I. Elder Abuse and the Courts 7 A. Elder Population Demographics and Elder Abuse 7 B. Elements of Elder Abuse 8 1. Abusive actions 2. Self-neglect 3. Financial abuse C. Dynamics of Elder Abuse 12 D. California's Approach to Addressing Elder Abuse 14 1. Elder Abuse and Dependent Adult Civil Protection Act 2. Adult Protective Services (APS) 3.
The individual's custodial sentence can range from a year in county jail to seven years in state prison. Penal Code 368 PC also includes fines ranging from $1,000 to $6,000. The exact fine or custodial sentence depends on how the elder was harmed and the extent of the injury. California elder abuse law also includes a timeframe in which you ...
1. abuse/neglect by another at home, 2. at an institution, or 3. self neglect. Elder abuse refers to an act or omission that results in harm or potential harm to the health or welfare of a person age 65 or older. It can include: State law on elder abuse often couples it with dependent adult abuse. A dependent adult is someone 18-64 who has ...
If the elder abuse or exploitation you observe is in relation to Medicare or Medi-Cal services, reach out to the Bureau of Medi-Cal Fraud & Elder Abuse Hotline at (800) 722-0432. There is also an elder abuse reporting form you can fill out online regarding Medi-Cal Fraud or elder abuse.